-
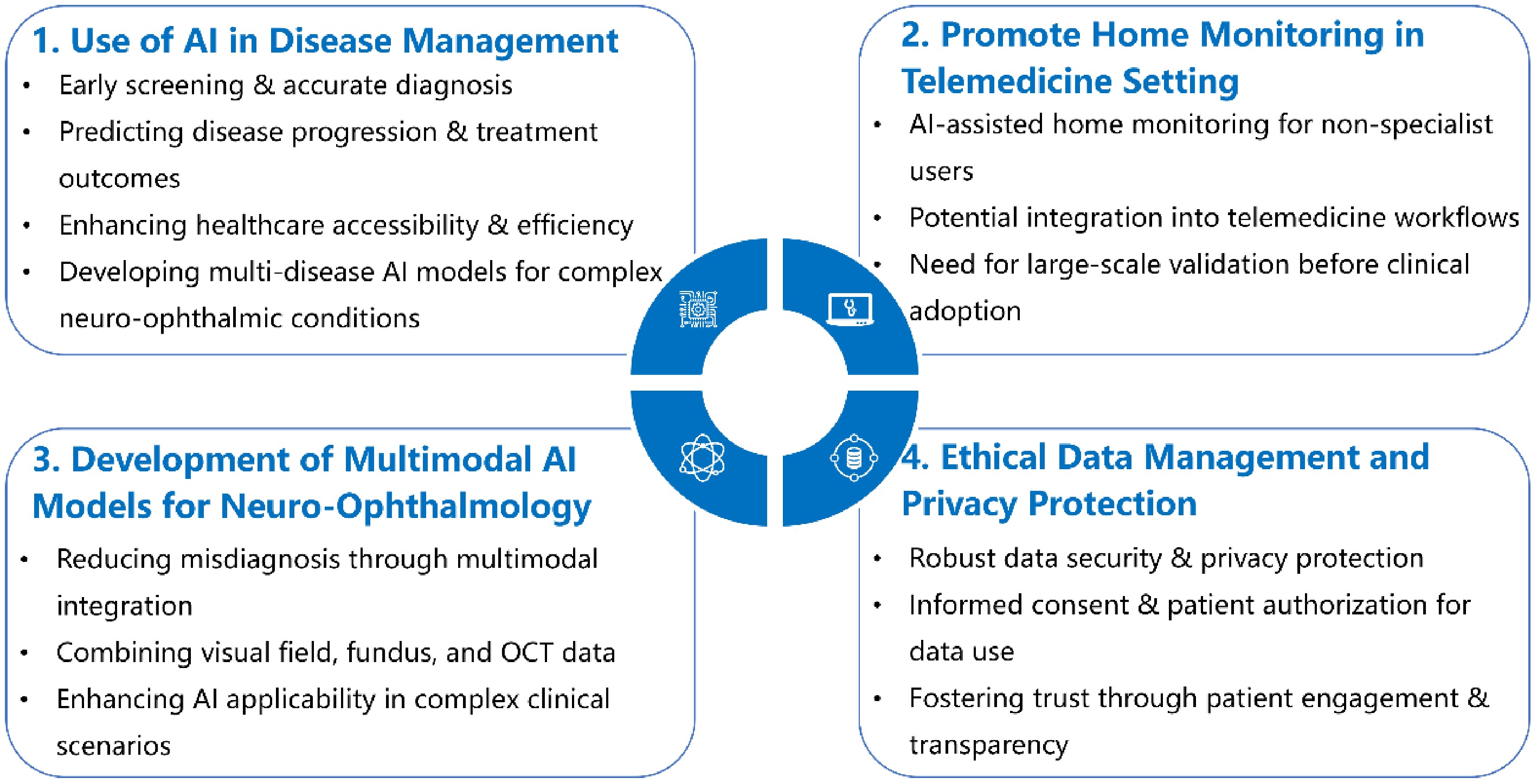
Figure 1.
Expert recommendations regarding the application of AI in neuro-ophthalmic diseases.
-
Neuro-ophthalmic diseases Artificial intelligence method Goals/predicted categories Result 1. ONH edema Akbar et al. Support Vector Machine Diagnosing/grading the severity of ONH An average accuracy of 92.86% for the classification of normal and papilledema images; an average accuracy of 97.85% for the classification of mild and severe papilledema images Ahn et al. CNNs and migratory learning methods Classifying photographs according to normal eyes, ONH edema, and pseudo-ONH edema Accuracy of more than 95.8% BONSAI consortium U-Net segmentation network and DensNet classification network Classifying ONH edema and other ONH abnormalities In the validation set, the system discriminated disks with papilledema from normal disks and disks with nonpapilledema abnormalities with an AUC of 0.9, and normal from abnormal disks with an AUC of 0.99; In the external testing dataset, the system had an AUC for the detection of papilledema of 0.96, a sensitivity of 96.4%, and a specificity of 84.7%. 2. Optic atrophy Yang et al. Automatic computer-aided detection Diagnosis of ONH pallor The fully automated CAD system achieved a sensitivity of 95.3% and a specificity of 96.7% for detecting optic disc pallor in color fundus images. The overall accuracy of the CAD system was 96.1%. Cao et al. GroupFusionNet Diagnosis of five optic neuropathies (anterior ischemic optic neuropathy, ONH edema, ONH inflammation, ONH vasculitis, and optic atrophy) GFN achieved a five-class classification accuracy of 87.82% on the test dataset. 3. Chronic glaucoma Li et al. DL system Detecting referable glaucomatous optic neuropathy In the validation dataset, this deep learning system achieved an AUC of 0.986 with sensitivity of 95.6% and specificity of 92.0%. Yang et al. CNN with a residual neural network architecture Distinguishing chronic glaucoma-like optic neuropathy from NGON The diagnostic accuracy of the ResNet-50 model to detect GON among NGON images showed a sensitivity of 93.4% and specificity of 81.8%. The area under the precision–recall curve for differentiating NGON vs. GON showed an average precision of 0.874. Li et al. ResNet-101-based DL method Detection of chronic glaucomatous optic neuropathy: confirmed chronic glaucomatous optic neuropathy, suspected chronic glaucomatous optic neuropathy, and normal eyes Accuracy: 94.1%; sensitivity: 95.7%; specificity: 92.9%; AUC: 0.992 for the identification of chronic glaucoma-like optic neuropathy and suspected chronic glaucoma-like optic neuropathy 3. Ocular motility disorders 3.1 Paralytic strabismus Almeida et al. Computer-assisted diagnostic system Diagnostic system for strabismus The method was demonstrated to be 88% accurate in identifying esotropia, 100% for exotropia, 80.33% for hypertropia, and 83.33% for hypotropia. Figueiredo et al. ResNet-50 as the neural network architecture Classifying the eye versions into nine positions of gaze Accuracy ranged from 42% to 92% and the precision from 28% to 84%, depending on the type of eye Zheng et al. DL method Screening horizontal strabismus in children Using five-fold cross-validation during training, the average AUCs of the DL models were approximately 0.99. In the external validation dataset, the DL algorithm achieved an AUC of 0.99 with a sensitivity of 94.0% and a specificity of 99.3%. Lu et al. Deep neural network Detection of strabismus in a telemedicine setting An accuracy of 93.9%, a sensitivity of 93.3%, and a specificity of 96.2% Jung et al. Active appearance model algorithm Detection of strabismus based on facial asymmetry An accuracy of 95% Chen et al. CNN models Identifying strabismus using eye movement tracking data Accuracy of 95%, a sensitivity of 94%, and a specificity of 96% Valente et al. Traditional computer vision methods Detecting exotropia An accuracy of 93.3%, a sensitivity of 80.0%, and a specificity of 100.0% 3.2 Nystagmus D'addio et al. Randomized samples and logistic regression trees Predicting visual acuity and ocular positional variability Coefficients of determination of 0.70 and 0.73 Wagle et al. DL system to collect data from video of eye movements Identify normal or at least two consecutive episodes of nystagmus The AUC, sensitivity, specificity, and accuracy were 0.86, 88.4%, 74.2%, and 82.7%, respectively. Kong et al. CNNs-LSTM Nystagmus Classifier Nystagmus pattern recognition Accuracy of 0.949 and an F1 score of 93.70% for nystagmus pattern classification; the accuracy of this classification network was 0.978 with an F1 score of 97.48%. 4. Other Neuro-ophthalmic Diseases Teh et al. Three-dimensional CNN Predicting the response of patients with painful diabetic peripheral neuropathy to lidocaine treatment AUC: 0.96; the F1 score was 0.95 in a validation experiment. Mou et al. DL method Grading the severity of nerve tortuosity An overall accuracy of 85.64% in four levels of grading Thomas et al. Back-propagation artificial neural network Visual field loss caused by pituitary tumors A sensitivity of 95.9% and a specificity of 99.8% CNNs, convolutional neural networks; AI, artificial intelligence; ONH, optic nerve head; AUC, area under the receiver operating characteristic curve; CAD, computer-aided detection; GFN, GroupFusionNet; DL, deep learning; NGON, non-glaucomatous optic neuropathy; LSTM, long short-term memory. Table 1.
Summary of current AI applications in the management of neuro-ophthalmic diseases.
Figures
(1)
Tables
(1)