-
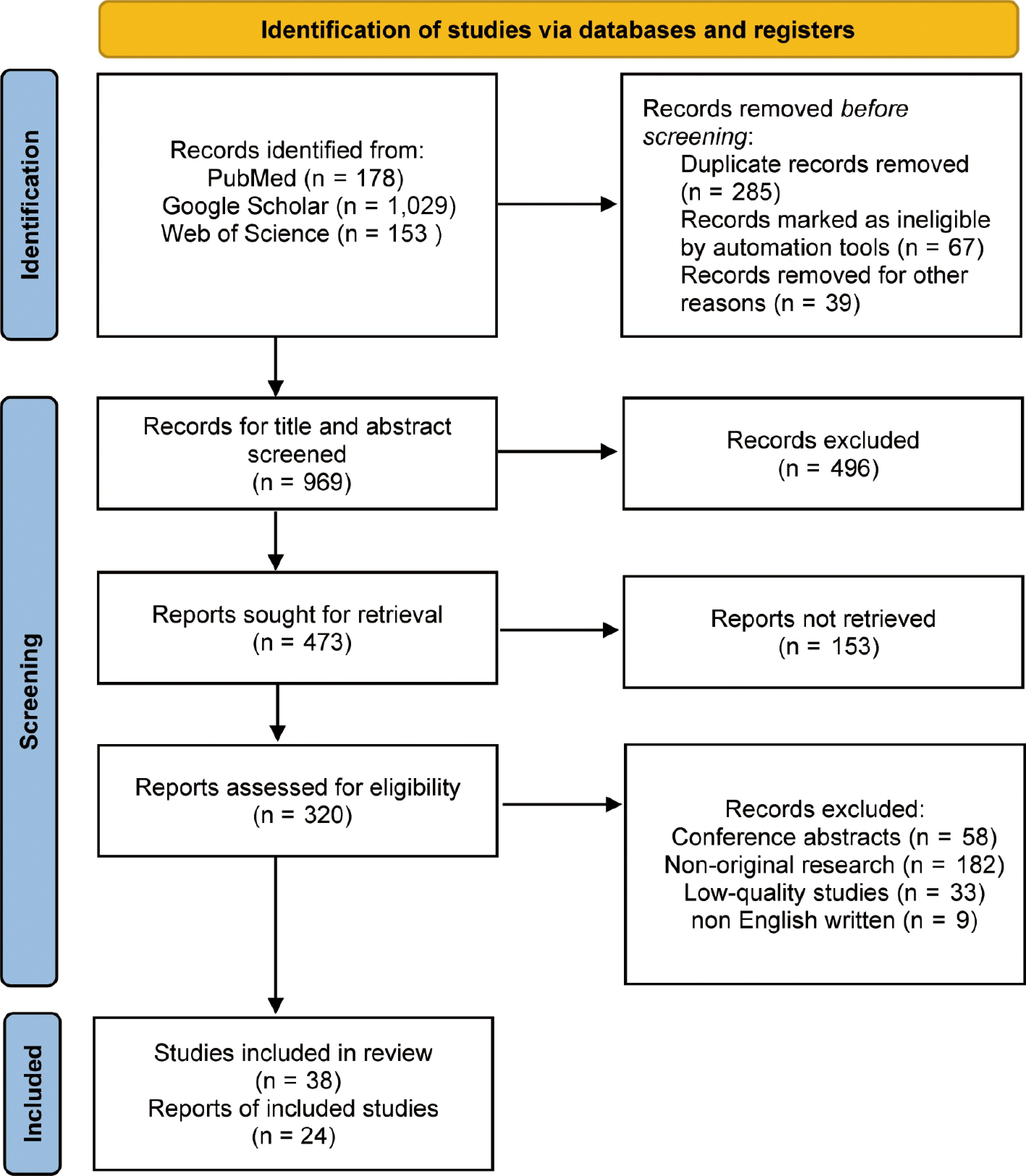
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 flow diagram for the systematic review, including searches in PubMed, Google Scholar, and Web of Science.
-
Figure 2.
The application of AI in clinical practice and AI literacy in ophthalmological education.
-
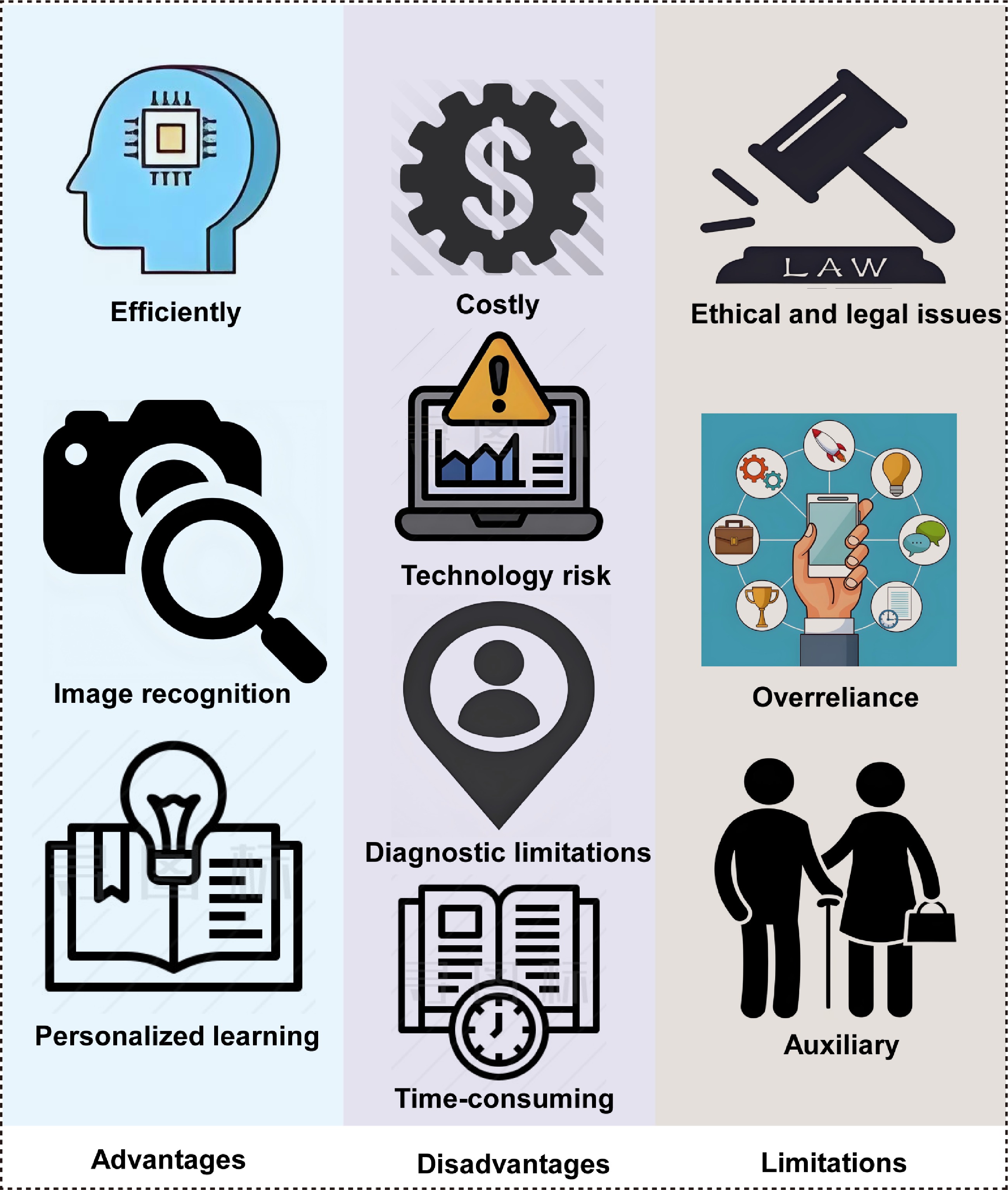
Figure 3.
The advantages, disadvantages, and limitations of AI in clinical and medical teaching applications in ophthalmology.
-
Training objective Trainees AI type AI educational role Key findings Key notes Publication AI-assisted problem-based learning (PBL) in ophthalmological education Medical students (clerkship) AI tutor system Empowering the learner Enhanced discussion efficiency and depth of understanding; students reported A positive learning experience Integration of PBL with AI-guided discussions Wu et al.[9] Training for identification of pathologic myopia Junior ophthalmology residents Image interpretation model with a feedback platform Support teaching AI-assisted feedback improved diagnostic accuracy and enhanced the quality of residents' reports AI-labeled images used as visual teaching aids Fang et al.[10] Personalized ophthalmology residency training Ophthalmology residents (all years) Recommendation system with adaptive learning pathways Support teaching Adaptive learning system improved the overall pass rate by tailoring content to individual weaknesses Real-time performance assessment used to dynamically adjust learning modules Muntean et al.[11] Enhancing AI literacy in medical imaging through a flipped classroom approach Undergraduate medical students (preclinical) AI-based flipped classroom and imaging tools Direct teaching Post-course AI literacy and confidence significantly improved in students Blending AI tools with flipped pedagogy to foster conceptual and applied understanding Laupichler et al.[12] Training for diabetic retinopathy grading using an AI reading label system Junior ophthalmology residents and medical students (clinical years) AI reading label system Direct teaching Improved grading accuracy and efficiency; fewer classification errors Structured training workflows with built-in performance monitoring Han et al.[13] Customized learning instructions and literature search using large language models (LLMs) Ophthalmology interns and junior residents LLM Empowering the learner Custom prompts and enhanced retrieval significantly improved literature comprehension, diagnostic reasoning, and self-directed learning efficiency Interactive dialogue, personalized guidance, and language generation for simulated clinical education Sonmez et al.[14] Training for manual diabetic retinopathy detection using an AI grading system Medical students and primary care providers Automated grading and feedback system Support teaching AI feedback reduced training time and lowered error rates by 20% Error flagging and performance tracking through AI-enhanced platforms Xu et al.[15] Training in surgical phase identification in cataract surgery videos Senior ophthalmology residents Video-based machine learning and deep learning Direct teaching Effective phase identification supports standardized procedural training Surgical phase data support structured training and feedback loops Yu et al.[16] Training in surgical instrument recognition in cataract procedures Cataract surgery fellows AI tool annotation model Support teaching Higher instrument recognition accuracy contributes to improved assessment of skills AI-generated annotations improve operative training and evaluation metrics Al Hajj et al.[17] Improving retinal disease recognition skills through training with synthetic images Medical students and beginner retina specialists Image-generative AI+ classification model Direct teaching Training with AI-generated images led to 40% improvement in recognition efficiency and reduced learning duration GAN-generated pathological images offer superior simulation-based training compared with traditional case studies Tabuchi et al.[18] Table 1.
Key empirical articles on AI in clinical education on ophthalmology (2019–2025).
Figures
(3)
Tables
(1)