-
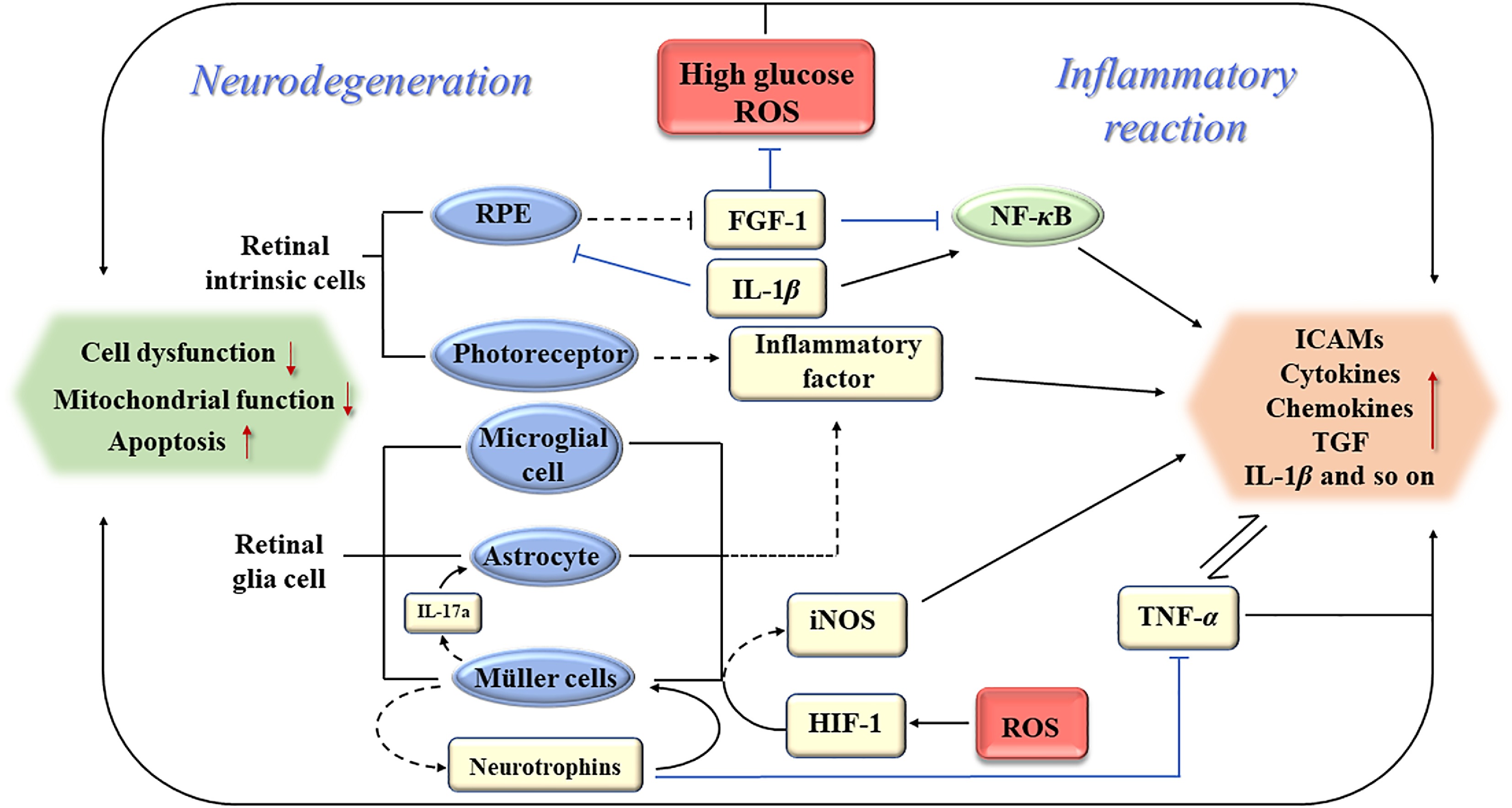
Figure 1.
Schematic of association between early inflammation and neurodegeneration of DR. RPE: retinal pigment epitheliums; ROS: reactive oxygen species; FGF-1: fibroblast growth factor-1; NF-κB: translocated nuclear factor kappaB; TNF-α: tumor necrosis factor-α; ICAMs: intercellular adhesion molecules; TGF: transforming growth factor; iNOS: inducible nitric oxide synthase; HIF-1: hypoxia-inducible factor-1.
-
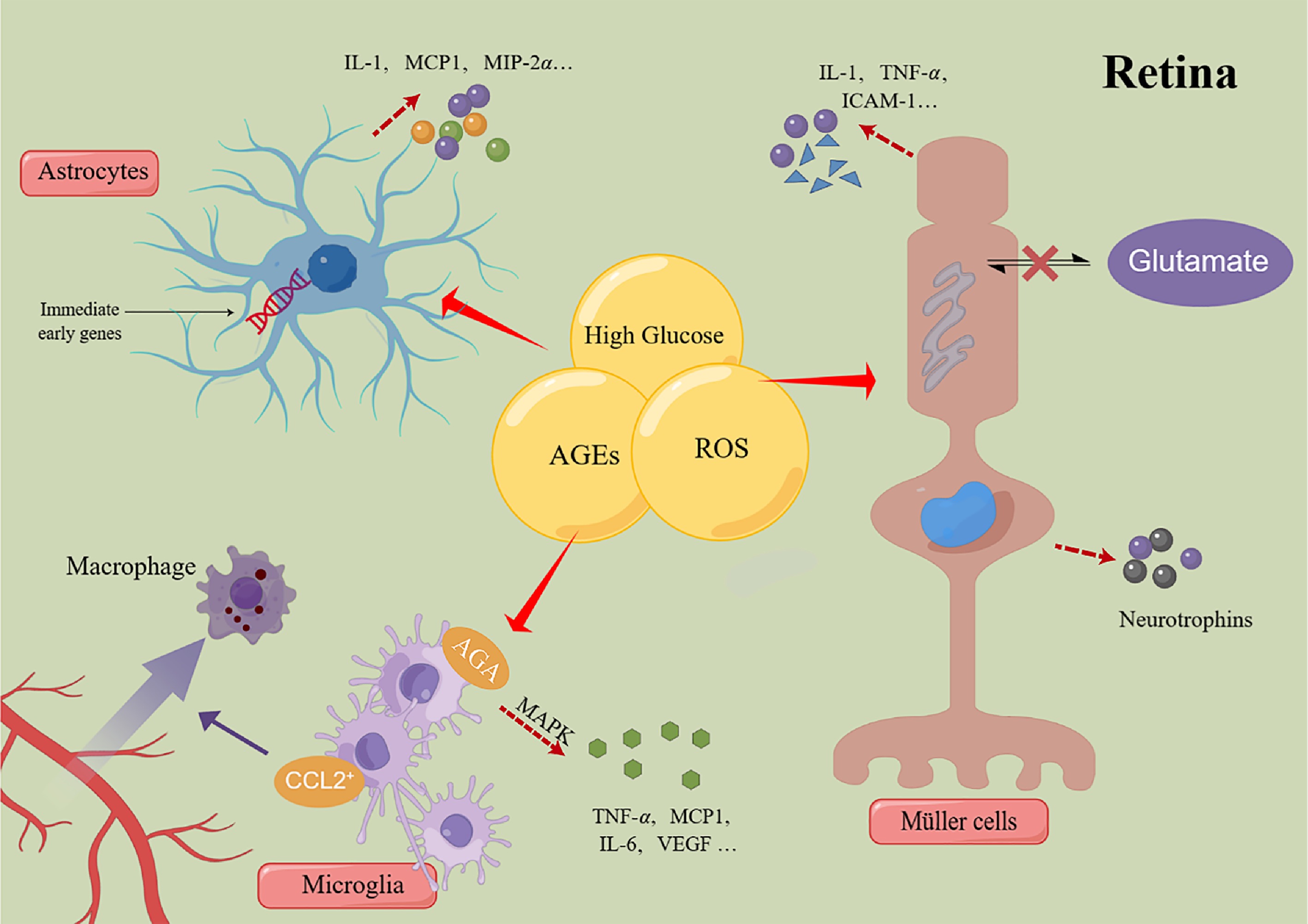
Figure 2.
Schematic of the mechanism of retinal glial cells regulating inflammatory response. MCP-1: monocyte chemotactic protein-1; MIP-2α: monocyte chemotactic protein-2α; TNF-α: tumor necrosis factor-α; ICAMs: intercellular adhesion molecules; CCL2: chemokine ligand-2; AGA: amadori-glycated albumin; MAPK: mitogen-activated protein kinase; VEGF: vascular endothelial growth factor; AGEs: advanced glycation end products; ROS: reactive oxygen species.
-
Detection means Advantages Disadvantages Key findings in DR Fundus microscopy and fundus photography · Criteria for clinical diagnosis and staging · Two-dimensional image · Microaneurysm · Widely usage · Internal retinal hemorrhage · Non-invasive · Intraretinal microvascular abnormality · Optic nerve and retinal neovascularization Dye-based fluorescein angiograph · Gold standard for visualization of vascular systems · Invasive · Microaneurysm · Assess the degree of vascular leakage · Long inspection time · Vascular leakage · Find ischemic areas · The effectiveness of the dye is affected by the disease itself · Non-perfused area · The deep capillary network structure is not well shown · Optic nerve and retinal neovascularization · Allergic reactions to dyes Optical coherence tomography · Non-invasive method for obtaining cross-section images · Vascular changes can't be shown · Macular edema · Gold standard for diagnosing DME and monitoring response to treatment · Retina thinning · Vitreous macular adhesion · Intraretinal cyst · Disorder of the inner retina Optical coherence tomography angiography · Deep resolution capacity (3D visualization) · Can't display vascular leakage · Microaneurysm · Non-invasive · Not widely used · Abnormal micro-vessels in the retina · Assess and monitor DR repeatedly · Neovascularization · Quantitative analysis · Quantification of microvascular changes in the retinal capillary network · Observe the microvascular system of retinal capillary plexus and choroid capillary ERG or mfERG · Early signs of retinal dysfunction · Can't show structural changes in the retina · The amplitude and a delay in the latency of the oscillatory potentials · Predict the development of early microvascular abnormalities Table 1.
Comparison of detection methods in DR.
-
Strategy Target New method Advantage Limitation Basic treatment Blood glucose, blood pressure, lipid concentration, and so on − Overall process The therapeutic effect is limited, and some patients still progress to PDR or DME Fundamental role Injection of medication VEGF New targeted drugs (such as Aflibercept and Faricimab) combined with PDEF, Ang, and other factors First-line therapy Applicable to late DR Delay the progression of DR Some patients have poor curative effect Improve visual acuity There is still a risk of cardiovascular complications Reduce the central retinal thickness Alleviate the resistance of monotherapy and vascular-related complications Inflammation Vitreous implants of sustained-release steroid drugs Activate glucocorticoid receptors to play a powerful anti-inflammatory effect It is suitable for DR Patients with poor anti-VEGF efficacy Reduce leukocyte stasis Second-line treatment Increased intraocular pressure, cataracts, and other adverse reactions Laser A thickened retina Pattern scanning lasers, micropulse techniques, and navigated laser system Improved accuracy Suitable for the late stage of DR, especially PDR Less collateral burn damage Risk of vision loss, and impaired night vision Gene therapy Pathogenic targets of DR, such as VEGF endostatin, angiostatin, HIF-1α, etc − Stable expression of treatment products Long-term treatment effects are still being studied Reduce complications from repeated injections Improve the structural parameters of the retina Table 2.
Comparison of current DR treatment methods.
-
Drug category Anti-inflammatory effect Protective mechanisms related to retinal neurodegeneration Nuclear factor erythroid 2-related factor 2 Regulate the expression of NF-κB and cyclooxygenase-2 Regulate the intracellular mitochondrial homeostasis Epigallocatechin-3-gallate Regulation of oxidative stress by down-regulation of the activity of ROS/thioredoxin Interaction protein/NOD-like receptor protein 3 inflammasome axis Reduce the reactive gliosis of Müller cells Resveratrol Diminish the accumulation of AGEs and attenuate the secretion of inflammatory mediators, including IL-1β, IL-6, TNF-α, and VEGF Inhibition of MicroRNA- 29b/specific protein 1 pathway to reduce Müller cell apoptosis Luteolin It primarily mitigates oxidative stress responses and the production of inflammatory mediators in retinal pigment epithelial cells via the SIRT1/P53 signaling pathway Inhibition of apoptosis of retinal ganglion cells and pigment epithelial cells Aldehyde reductase inhibitors Suppress the phosphorylation of extracellular signal-regulated kinase 1/2 as well as the expression of NF-κB and VEGF Alleviate the injury of retinal ganglion cells, yet there is a deficiency of specific preparations. Sodium-glucose cotransporter-2 inhibitors Enhance the management of retinal oxidative stress and attenuate the levels of inflammatory factors Mitigate cellular edema and loss in the vicinity of the optic nerve head Table 3.
Therapeutic drugs for DR have overlapping mechanisms in anti-inflammation and improving neurodegeneration.
Figures
(2)
Tables
(3)