Introduction: Molecular targeting drugs are recommended as second-line treatment for intrahepatic advanced hepatocellular carcinoma (HCC). However, in Asia, hepatic arterial infusion chemotherapy (HAIC) is also considered as a second-line treatment because it improves the survival of responders. The aim of this study was to predict responders and non-responders to HAIC with low-dose cisplatin plus 5-fluorouracil (LFP) using tumor markers.
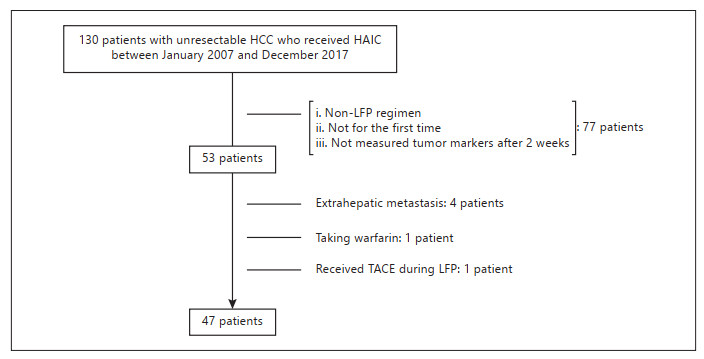
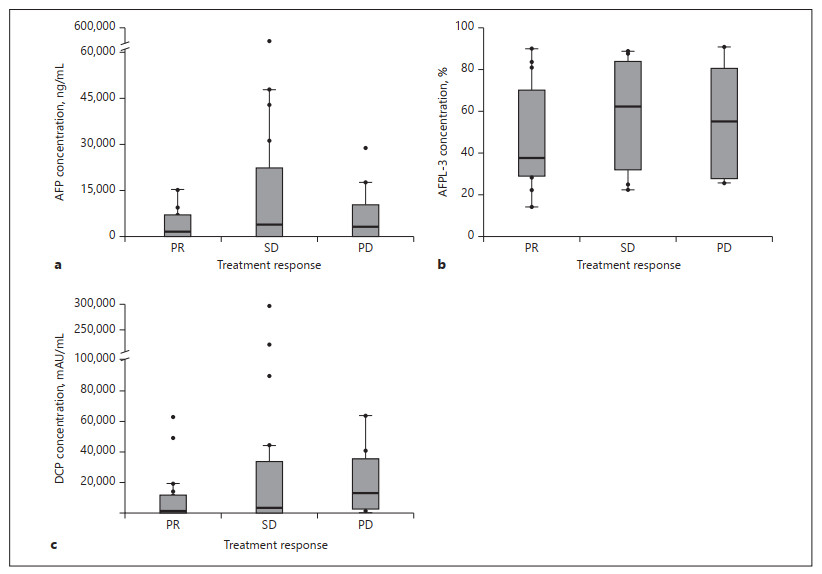
Objective and Methods: The data of 47 patients who received LFP for the first time in our hospital were analyzed retrospectively. We evaluated the association between treatment response by Response Evaluation Criteria in Solid Tumors and the changing ratio of the serum concentration of α-fetoprotein (AFP), Lens culinaris agglutinin-reactive fraction of AFP (AFP-L3), and des-γ-carboxy prothrombin (DCP) 2 weeks after LFP initiation.
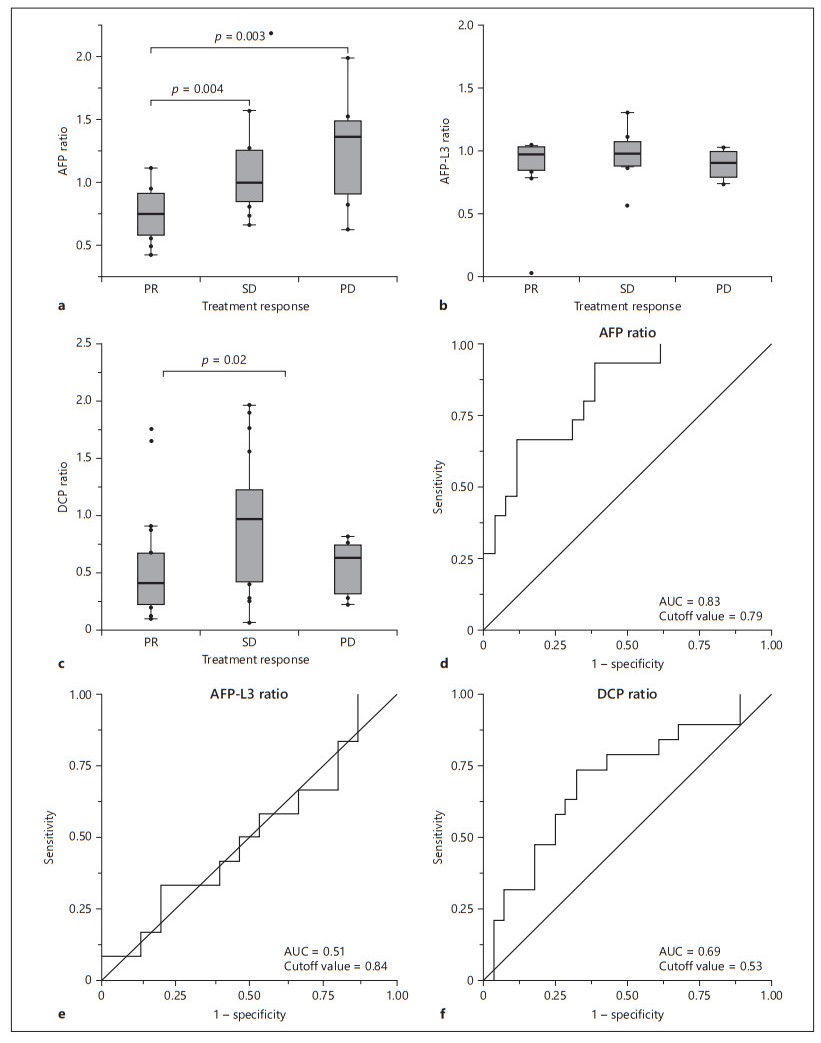
Results: The number of patients showing a complete response (CR), a partial response (PR), stable disease (SD), and progressive disease (PD) was 0 (0%), 20 (43%), 18 (38%), and 9 (19%), respectively. The AFP ratio showed significant positive correlations for PR vs. SD (p = 0.004) and PR vs. PD (p = 0.003). The DCP ratio correlated significantly for PR vs. SD (p = 0.02). The optimal cutoff values for responders were 0.79 for the AFP ratio and 0.53 for the DCP ratio. Prediction using both or either cutoff value showed 93% sensitivity, 53% specificity, a 94% negative predictive value, and a 57% positive predictive value.
Conclusion: Optimal cutoff values for AFP and DCP ratios enable prediction of nonresponders to HAIC with LFP. This simple and early assessment method allows the use of HAIC and molecular targeting drugs for HCC treatment.