-
According to a report by the World Health Organization (WHO), there are over 1 billion individuals worldwide who use tobacco, making the tobacco epidemic one of the most critical public health concerns[1]. China is the most populous country in the world, and its tobacco consumption accounts for 44% of the global total. The resulting health issues have brought about significant economic and social burdens[2]. Tobacco dependence is widely recognized as a substantial obstacle to smoking cessation in cases of nicotine addiction[3]. Current estimates indicate that approximately 183.5 million individuals in China are active smokers with nicotine dependence, regardless of gender[4].
The Chinese government has implemented a range of measures in recent decades to support smoking cessation. In 2005, China became a signatory to the World Health Organization's Framework Convention on Tobacco Control (FCTC)[5]. Furthermore, in 2014, the National Health and Family Planning Committee introduced the first nationwide regulation for banning smoking in public spaces, which stipulates that smoking is completely prohibited in indoor public places, indoor workplaces, and public transportation, providing legal protection for public health[6]. Additionally, China has established tobacco control agencies at various levels and devised a series of policies and measures aimed at promoting smoking cessation. These include raising tobacco taxes, providing comprehensive smoking cessation services and support programs, as well as strengthening regulations pertaining to tobacco advertising and sales[7]. Smoking behaviors are influenced by both physiological factors[8], such as nicotine dependence, and psychological factors[9] including emotions and cognitive perceptions of smokers. Therefore, the barriers faced by quitters encompass not only the physical addiction to nicotine but also emotional aspects, external environment influences, and social surroundings. China's unique social and cultural context impacts smoking behavior and cessation efforts. In Chinese society, smoking has long been deeply ingrained in social norms and customs, it is often associated with masculinity, social status, and interpersonal relationships[10]. Furthermore, China's vast population size and diverse socioeconomic backgrounds contribute to the complexity of implementing effective smoking cessation strategies. Factors like education level, occupation type, income disparities, and regional differences may influence individual attitudes towards smoking as well as their behaviors[11,12].
In recent years, there has been a growing global concern regarding adolescent smoking[13], as it not only presents immediate health risks but also escalates the likelihood of long-term tobacco addiction[14]. Furthermore, extensive research has unveiled multiple factors that contribute to adolescent smoking, including anxiety, stress, peer influence, familial smoking habits, and easy access to tobacco products[15,16]. In light of the detrimental effects of smoking during adolescence, several strategies have been devised to address youth smoking and promote cessation. These intervention approaches encompass incentives, school-based programs, and advertising restrictions[17]. Despite these concerted efforts made thus far, the prevalence of adolescent smoking in China remains a significant public health issue[18], underscoring the necessity for further investigation into youth tobacco use.
This study aimed to investigate the barriers and facilitators of smoking cessation among Chinese smokers using semi-structured qualitative interviews based on the Behavior Change Wheel (BCW) theory[19]. Qualitative research in smoking cessation enables us to analyze smokers' cognition, experiences, attitudes, and beliefs, as well as observe their smoking behavior and willingness to quit. By gaining insights into external factors that influence smokers through qualitative research and combining them with smoking cessation interventions, we can enhance the success rate of quitting. Additionally, this study explores how to prevent and control adolescent smoking by considering advice and experiences from current and past smokers across different age groups regarding youth smoking initiation.
-
The present qualitative study adhered to the Consolidated Criteria for Reporting Qualitative Research (COREQ)[20], ensuring rigorous reporting standards. Additionally, ethical approval was obtained from the Medical Ethics Committee of Beijing University of Chinese Medicine (No. 2021BZYLL03010).
Study setting and participants
-
The collection of participants' demographic details and smoking history was conducted through semi-structured recorded interviews, with interview durations ranging from 20 to 35 min. In response to the COVID-19 pandemic, some interviews were carried out online using Tencent meeting software (version 2.8.1.200), while others were conducted as face-to-face interviews in Beijing, China. The development of both the research protocol and the preliminary interview outline was finalized during the period from December 2020 to February 2021.
The snowball sampling approach, primarily relying on referrals through social networks and acquaintances, was applied to generate a diverse and convenient sample of smokers or ex-smokers across various age groups and occupational backgrounds. While the typical size of qualitative interviews is 10−15 participants[21−23], our objective was to conduct interviews with a minimum of 15 participants to ensure data saturation.
We recruited individuals aged 12 to 70 years who were current or former smokers with a smoking history of at least six months. Participants were required to provide informed consent and be willing to undergo audio recording during the study. Exclusion criteria encompassed self-reported respiratory diseases, such as chronic obstructive pulmonary disease or asthma within the past year. Additionally, participants unable to complete the interview due to personal reasons were excluded.
Data collection
-
The study commenced by obtaining informed consent from all participants, with those under the age of 18 years requiring consent from their legal guardians. Thirty semi-structured interviews were conducted by a team of three researchers. The interviews were led by a male postgraduate student holding a master's degree, who had prior experience in conducting interviews related to smoking (SY Q). Transcripts of the interviews were generated by CL L (female, PhD) and XH L (female, PhD). All researchers had received comprehensive training in interview techniques and possessed previous involvement in qualitative research.
Before conducting the interviews, participants were provided with an interview schedule by the interviewer. Additionally, all participants were requested to provide essential demographic information, including age, gender, relationship status, fertility status, age at initiation of tobacco consumption, duration of tobacco use (in years), frequency and quantity of tobacco consumption, self-perceived level of addiction, number of quit attempts made previously, and history of respiratory disease.
The interview outline was developed based on predetermined themes derived from previous research[24−26]. Pilot interviews were initially conducted with 2−3 potential participants to refine the interview outline and incorporate additional questions (refer to Table 1). Subsequently, more in-depth questions were posed based on participants' responses. The interviews were recorded audibly, and automatic transcripts were generated using iFLYTEK Voice Recorder. Participants were then allowed to review and provide feedback on their interview transcripts. An iterative approach was employed to ensure data saturation.
Table 1. Interview outline and additional questions.
Question outline Additional questions/prompts Could you tell me the reason why you started smoking in the first place? ● Does anyone smoke in your household?
Yes. → Do you think family influence is related to your start of smoking?
No. → What affected you to start smoking mainly?
● Under what circumstances made you more prone to smoking? (such as time points or scenes)
● Why do you think these situations make it more likely for you to smoke? Have these been an obstacle to quit?
● Is it possible to avoid these situations?What do you think about stopping smoking? ● Do you think nicotine dependence is a condition that needs treatment? And why? How do you feel physically and emotionally when you abstain from smoking?
● If quitting smoking is not mandatory for you, would you still like to quit smoking? (Or, what are the reasons for the necessity to quit smoking?)
● (With smoking cessation experience(s)) Could you tell me about your considerations or motivations for each attempt? What effects did they have?
● (With no smoking cessation experience) Would you consider quitting smoking in the future? Under what circumstances will you quit/restart smoking?
● Which factors do you believe provide you with more confidence in quitting smoking, intrinsic or extrinsic factors? Intrinsic factors such as concerns for health conditions or personal images. Extrinsic factors such as opposition from families, concerns for others' health, or relevant regulations that make smoking inconvenient.
● (Have health issues) How has smoking affected your issues? Would you be willing to quit smoking for the sake of your health?What are your perceptions of the harm and danger associated with smoking? ● (For example, secondhand smoke, effects on the lungs, effects on fertility)
● Are you aware of any harmful substances that enter the body through smoking? (Such as nicotine, tar, sulfur monoxide, carbon monoxide, and others)
● Could you tell me about the diseases caused by smoking?
● Have you attended any seminars or public lectures on the dangers of smoking? (For example, community lectures, slogans, advertisements). How did these experiences make you feel?What methods have you tried to quit smoking? ● Do you think those methods were effective? To what extent did they help you? Could you list some approaches that you have heard of but have not yet tried? Why haven't you tried them?
● Do you think mindfulness therapy, acupuncture, traditional Chinese medicine can help with smoking cessation?
● Have you ever tried any traditional Chinese medicine methods to help quit smoking?
Yes. → What did you try and how do you feel about it?
● Do you have any partners or friends who supported you during your smoking cessation journey?
● Have you heard of smoking cessation clinics?
Yes. → How did you learn about them? Have you ever visited a smoking cessation clinic for consultation or treatments?
If yes, could you share with me more about your experience?
No.→Would you consider visiting a smoking cessation clinic in the future?
If no, what were the reasons for not seeking help from the clinics?
● Have you ever used e-cigarettes?
Yes. → Could you tell more about your experience of using them and whether they helped you in any way? Do you think that e-cigarettes are equivalent to regular cigarettes? Can e-cigarettes replace regular cigarettes, and why do you think so?
● In your opinion, which is more crucial for quitting smoking, determination or method?What do you think are the most important factors to succeed in quitting smoking? ● Which factor do you consider the most essential for yourself? Why?
● To achieve smoking cessation successfully, what type of assistance or support do you need throughout the process?
● Has the coronavirus disease 2019 (COVID-19) pandemic and its consequences influenced your attempts to quit smoking or your smoking behavior?
● What do you think regarding teenage smoking issues? Do you have any advice to prevent teenagers from smoking?Data analysis and theoretical framework
-
The Behavior Change Wheel (BCW) theory, derived from a systematic review of behavior change interventions, is widely employed for behavioral interventions[19,27−30]. It identifies four core categories - capability, opportunity, motivation, and behavior (COM-B model), providing a systematic framework to understand and explain key factors of behavioral change. Therefore, it offers valuable insights into smoking cessation and smoking behavior to achieve the goal.
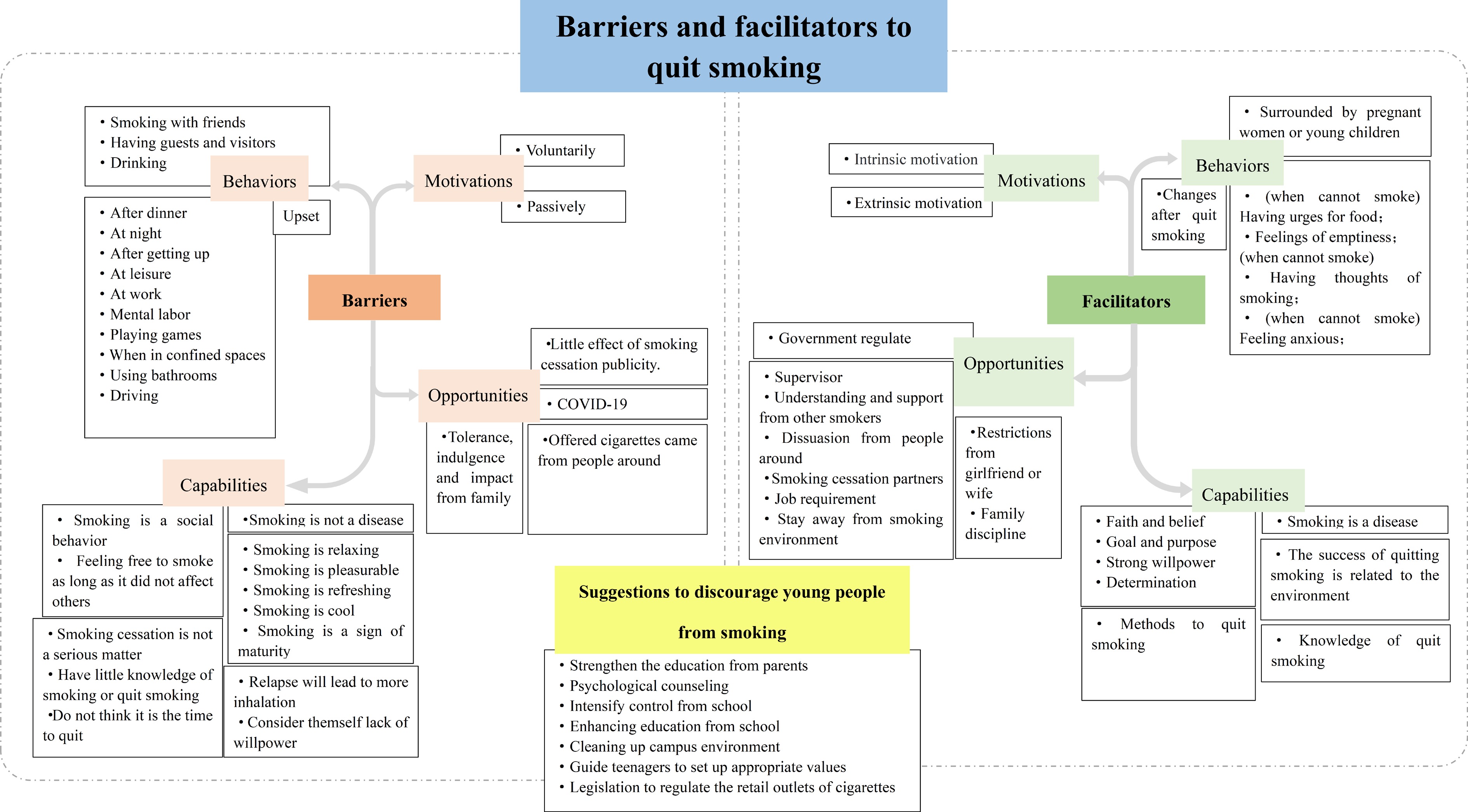
Based on the COM-B model, we employed Framework analysis to synthesize the smoking behaviors associated with barriers and facilitators of smoking cessation. The four pre-established themes encompass capability, opportunity, motivation, and behavior. To further investigate factors influencing smoking cessation implementation in the early stages, this study included adolescent smokers and conducted a separate examination of barriers and facilitators specific to teenage smoking cessation. Behavioral orientations encompassed both continued smoking and smoking cessation. All transcripts were imported into Nvivo12 (Version No. 12.6.0.959) for code generation and theme analysis management.
-
Between January 2021 and February 2021, a total of 31 eligible participants were identified for the study. All participants provided consent and agreed to participate and completed their interviews without any refusals or interruptions. One participant who initially agreed to participate but subsequently refused to be recorded and was excluded from the study, all data on this participant was destroyed. The analysis included interviews of 30 participants, comprising 25 males and five females, who were from five different cities in China. The age of participants ranged from 13 to 63 years, with tobacco consumption starting as early as 8 years old and the oldest age of smoking initiation being 37 years. The duration of smoking ranged from 1 to 40 years, with an average of 18.15 years. A summary of the characteristics of the included participants are reported in Table 2.
Table 2. Summary of basic demographic information on 30 interviewees.
Items Characteristics No. of participants (%) Gender Male 25 (83.3) Female 5 (16.7) Age (years) < 18 3 (10.0) ≥ 18 and ≤ 45 21 (70.0) > 45 and < 60 3 (10.0) ≥ 60 3 (10.0) Occupation Designer 3 (10.0) Lawyer 1 (3.3) Teacher 5 (16.7) Business manager 1 (3.3) Host of live RPG 1 (3.3) Student 6 (20.0) Civil servant 7 (23.3) Police 2 (6.7) Energy industry worker 1 (3.3) Ex-soldier 1 (3.3) Doctor 1 (3.3) Housewife 1 (3.3) Relationship status Dating 7 (23.3) Single 9 (30.0) Married 13 (43.3) Fertility status Have children 12 (40.0) No children 17 (56.7) Planning to have children 1 (3.3) Age of the first TC < 18 21 (70.0) ≥ 18 and ≤ 45 9 (30.0) Years of TC < 10 12 (40.0) ≥ 10 18 (60.0) Frequency of TC* Everyday 17 (56.7) Occasionally 4 (13.3) None 9 (30.0) Desire to smoke Yes 17 (56.7) No 4 (13.3) Quit 9 (30.0) No. of TC ≤ 5 cigs/d 7 (23.3) > 5 and ≤ 10 cigs/d 6 (20.0) > 10 cigs/d 11 (36.7) It depends 1 (3.3) E-cigs 1 (3.3) No. of attempts to quit smoking Never 13 (43.3) ≤ 3 14 (46.7) > 3 and ≤ 5 1 (3.3) > 5 and ≤ 10 1 (3.3) > 10 1 (3.3) Partners quit smoking / 13 (43.3) Yes 5 (16.7) No 12 (40.0) Experiences of e-cigarette use Yes 21 (70.0) Never 9 (30.0) No., Number; RPG, role playing game; TC, tobacco consumption. * The frequency of smoking in the past month. Additional details regarding the 30 included interviewees are provided in Supplementary Table S1.
The transcripts yielded a total of 193 codes from 78,881 Chinese words. To comprehend the barriers and facilitators to smoking cessation, we analysed the barriers using all combinations of codes related to 'continue to smoke' and the facilitators using all combinations of codes related to 'stop smoking'. Where possible, the content extracted from the interviews was then integrated into the four predetermined themes: capability, opportunity, motivation, and behavior, which represent the four components of smoking and smoking cessation according to the BCW theory). Furthermore, a new theme emerged: 'suggestions for preventing teenagers from starting smoking'. Refer to Fig. 1 for the primary and secondary codes. Examples of the transcribed text of the codes are shown in Supplementary Table S2.
Barriers to smoking cessation
Capabilities
-
Psychological capabilities encompassed individuals' perspectives on smoking. As for physical capabilities, changes in health conditions exerted an impact. Most participants agreed that smoking was a hobby, habit, social phenomenon, or recreational activity, and they didn't realize that smoking addiction was a chronic disease. Many participants had limited knowledge about the hazards of smoking, including both the toxic chemical components present in cigarettes and the spectrum of smoking-related diseases.
'I don't think so. I think it's a kind of entertainment. It's not so serious that needs to be treated with medical approaches.' (016-male-15 yrs)
'I don't know much about it. I have heard of a substance called 'nicotine''(021-male-56 yrs)
In terms of awareness, young participants perceive quitting smoking as unnecessary at their age, while older participants believe that quitting smoking at an advanced age is too late.
'It's just, from my own point of view, I recognize that quitting smoking is beneficial, but I didn't take it very seriously.' (002-male-27 yrs)
'"I feel that it doesn't matter if I quit or not at this age. I just smoke a bit less. It's fine to not smoke once in a while.' (030-female-61 yrs)
Some participants lacked confidence in their ability to quit smoking. Two participants mentioned that their smoking addiction became worse after unsuccessful cessation attempts.
Opportunities
-
Social influence appeared as a crucial factor in shaping opportunities. Government regulations and the COVID-19 pandemic also had an impact. Approximately one-third of the participants believed that family influence significantly contributed to smoking behavior. The family's acceptance and permissiveness towards smoking made them to initiate and maintain this habit. Some participants mentioned that people around them would hand them cigarettes, and this made it difficult to refuse.
Most participants reported that smoking cessation slogans or picture publicity did not affect them. They believed that the content exaggerated reality, leading them to consciously avoid or forget the messages.
'To be honest, I didn't feel anything. When I purchase the cigarettes, there's no point in putting anything on them. I already bought them, didn't I?' (006-female-21 yrs)
In addition, a small proportion of participants reported that COVID-19 had also impacted their smoking behavior. One participant mentioned decreased tobacco consumption increased due to staying at home during the pandemic.
'Well ... more (smoking), more likely to smoke. I think it's easier than ever because I'm staying at home for so much time.' (004-male-28 yrs)
Motivations
-
The motivations to continue smoking can be categorized as voluntary or passive. Participants were motivated to smoke because of their curiosity about tobacco, the need for stress relief, to kill time, and to combat boredom. Some participants also mentioned that smoking could enhance their relationships and serve as a crucial social channel. Participants were exposed to passive smoking due to the influence of smokers around them and their exposure to others' existing smoking habits.
'The first time I smoked, well, I suppose it was out of curiosity. There were no specific reasons. One of my brothers was smoking, then I started smoking after him.' (012-male-46 yrs)
Behaviors
-
Many participants considered smoking a social activity. Smoking with friends, having guests and visitors, and engaging in social interaction, with or without alcohol, further reinforced the participants' smoking behavior.
Smoking habits were intertwined with daily activities, including post-dinner, nighttime, morning, leisure, work, stress relief, gaming, enclosed space, restroom use, and driving.
'I have developed a habit of smoking after waking up and after meals.' (011-male-28 yrs)
Psychologically, several participants believed that smoking relieved their stress, reinforcing their continued smoking habit.
'It's kind of like the thought of releasing one's stress. It's sort of an adult-way of preventing meltdowns (laugh).' (004-male-28 yrs)
The withdrawal symptoms associated with tobacco dependence frequently induce psychological distress, with interviewees commonly experiencing heightened anxiety and restlessness when experiencing the urge to smoke in situations where smoking is not possible.
'Mostly, I'm feeling anxious. Otherwise, it's okay. If there was really no cigarette, it's actually okay. It (the feeling of anxiety) will pass after a while. But it sucks when I'm trying to look for cigarettes.' (001-male-23 yrs)
Facilitators of smoking cessation
Capabilities
-
For psychological capabilities, participants emphasized the importance of their perspectives on the nature of smoking and self-psychological intervention. According to seven participants, they believe that nicotine dependence is a disease that also impedes successful smoking cessation efforts.
'I consider it a disease, because there is an addictive behavior. I don't think it as fundamentally differ from the drug addiction. Quitting without external requirements is challenging, and the cessation process can be highly uncomfortable.' (027-male-25 yrs)
Over half of the participants recognized strong willpower and self-control as essential factors for successful cessation. Approximately two-thirds of the participants attempted to quit smoking unassisted. Some participants emphasized the importance of setting goals in advance.
Regarding physical capabilities, acquiring a broader range of cessation methods and knowledge can assist smokers in their cessation efforts. One participant, who was currently using nicotine replacements, reported feeling dizzy and nauseous due to excessive usage. Although five participants had heard about smoking cessation clinics, none had ever visited cessation clinics for assistance, and it was not even clear whether there were such clinics in China. The limited awareness and understanding of smoking cessation clinics had resulted in the underutilization of this potentially effective smoking cessation intervention. One participant expressed a willingness to consider seeking treatment at a clinic if they were unable to quit smoking on their own.
'I read a book about it. But I don't know if it exists in China. If there is, I would love to give it a try if I failed by myself.' (018-male-34 yrs)
For other smoking cessation methods, cigarette tapering (reducing gradually), snacks, complementary, and alternative therapy were commonly mentioned. Four participants believed that gradually reducing the number of cigarettes would be an effective approach. Approximately one-third of the participants mentioned using snacks such as nuts, gum, and potato chips as a strategy to quit smoking. Some participants believed that traditional Chinese medicine could be effective. One participant reported that his colleague experienced nauseous and sickness when exposed to the smell of smoke after using acupoint embedding as a smoking cessation method. Three participants suggested that Chinese herbal medicine and acupuncture might serve as potential aids for cessation. Additionally, several participants also mentioned behavioral methods, exercise and various other smoking cessation methods.
Opportunities
-
For some participants, family supervision and companionship were beneficial in their cessation efforts.
'When it comes to quitting smoking, it's because of the people around me, whether they are children or parents, as they can also influence you to quit.' (025-male-39 yrs)
'I feel like I need someone watching me all day. I can't do this on my own.' (001-male-23 yrs)
Some participants emphasized the crucial role that other people could play in their cessation processes. For example, supervision, others dissuading them, understanding and support from fellow smokers, and the influence of partners to quit smoking together. Certain participants acknowledged that public awareness and government regulations could be helpful in promoting cessation.
Four participants reported a slight reduction in their cigarette consumption during the COVID-19 pandemic due to reduced socializing opportunities, increased mask-wearing, and a desire for better health.
'It does have a little effect, because of the need to wear a mask, it is not convenient to smoke. So I smoked relatively less cigarettes' (022-male-27 yrs)
Behaviors
-
Some participants refrained from smoking when they were near pregnant women or young children, while others experienced an increased appetite after quitting, which helped release the feelings of emptiness and anxiety commonly associated with cessation.
Analysis of interviewee narratives revealed that both the health improvements resulting from successful smoking cessation and the supportive attitudes of family and friends generated significant positive psychological outcomes for the participants. Two individuals who successfully quit smoking described experiencing mental and physical improvements.
'After I quit smoking, my coughs disappeared, and people no longer disliked me for the smell of cigarettes on me.' (029-male-63 yrs)
'It is evident that my sense of taste has returned, and my sense of smell has become more sensitive since I stopped smoking.' (007-male-24 yrs)
Motivations
-
Motivations for smoking cessation among interviewed participants could be divided into two categories--internal factors and external factors. Some participants reported they were motivated to quit because they were concerned about their own and their family's health, plans to have children and personal appearance. Two young female participants expressed that preparing for pregnancy would be a significant motivating factor for them to quit smoking. Two young male participants mentioned that they would attempt to quit smoking when their partner was preparing for pregnancy.
'I might consider quitting when I'm trying to get pregnant.' (010-female-26 yrs)
Some participants quit smoking out of concern about their appearance.
'And now, with the increase in people's education levels, many individuals try to avoid me when I'm smoking. This feeling sucks.' (027-male-25 yrs)
As for objective factors, the motivation to quit smoking arose from health issues associated with tobacco usage, public environment restrictions, and the economic burden.
'Mainly because I don't believe my body condition was healthy anymore. My blood pressure increased.' (012-male-46 yrs)
Suggestions to discourage young people from smoking
-
Many participants advocated for stricter regulations at the point of sale, such as age verification of 18 and stronger market regulations for tobacco industries. The majority of participants noted that young people are highly susceptible to the influence of the family and school environment, which can lead them to initiate smoking. One participant mentioned that school teachers guided him away from tobacco use.
'My father and brother are both smokers and I became curious about cigarettes. If they didn't smoke, I probably wouldn't have tried it.' (009-female-13 yrs)
'When I smoked for the first time, my high school teachers and coaches discovered it, and they provided me with essential education that strengthened my resolve to quit.' (015-male-18 yrs)
Two participants also suggested seeking more suitable ways to relieve stress for adolescents instead of smoking. They emphasized the importance of providing alternative outlets for stress management that are healthier and more constructive.
-
In this study, we identified four major themes based on the pre-set framework. The synthesis of the study revealed that smoking cessation outcomes were influenced by two behavioral modes: weakening smoking incentive motivation, capability, and opportunity aspect, while reinforcing beliefs related to quitting from these same aspects. In addition, we explored the potential approaches regarding how to discourage young people from consuming tobacco.
Capabilities
-
Capability includes relevant knowledge required for smoking and smoking cessation. Increasing smokers' awareness of the hazards of tobacco use is vital, which may also increase their motivation to change their behavior. In the 2018 China Adult Tobacco survey report, 82.8% of people knew smoking could lead to lung cancer, 50.8% knew about heart disease, 41.4% heard about stroke, and 26% were aware of erectile dysfunction[31]. The perception of one's health condition is also a major factor influencing smokers' willingness to quit.
Intriguingly, our study also found that older smokers perceive quitting smoking as too late, and younger smokers perceive it as too early. Older smokers may have been smoking for a longer duration and might have attempted to quit in the past. They may feel discouraged or resigned to the habit, believing that quitting at their age would not significantly improve their health. Younger smokers, on the other hand, may not feel the immediate urgency to address their smoking habits. The divergent perceptions of older and younger smokers regarding the timing of quitting smoking provide valuable insights into the challenges and considerations for smoking cessation interventions. Previous studies[32,33] have shown that the earlier the time to quit smoking, the greater the benefit, so it is meaningful to carry out smoking cessation education for smokers of different ages and popularize the correct concept of quitting smoking time to promote smokers to quit smoking.
Capability also encompasses the resources of smoking and support of smoking cessation. China's inaugural smoking cessation clinic was established in Beijing in 1996. According to data from the Chinese Center for Disease Control and Prevention, the number of such clinics nationwide has grown to 234 as of 2020[34]. However, significant regional disparities and inadequate public awareness campaigns have resulted in persistently low recognition and utilization rates of these facilities[35]. To address these challenges, future initiatives will focus on integrating smoking cessation services with community health centers to enhance accessibility. Concurrently, more leverage digital platforms to establish online smoking cessation clinics, thereby expanding their visibility and outreach. These combined efforts aim to provide more comprehensive and accessible support systems for individuals pursuing smoking cessation. While current research indicates the potential benefits of traditional Chinese medicine (TCM) in smoking cessation interventions, public awareness remains limited. Present studies predominantly concentrate on acupuncture as a treatment modality[36]. Future investigations into Chinese herbal interventions could significantly contribute to the development of comprehensive strategies for aiding smoking cessation.
Such as smokers require financial resources to purchase cigarettes. A cross-sectional study conducted in China reported that an estimated 80.5% of youth smokers purchased cigarettes in the past one month, and this study revealed that strengthening laws to protect minors and prohibiting the sale of tobacco products may contribute to youth tobacco control[37]. It is noteworthy that many participants also strongly expressed that the control and enforcement measures on the sale of tobacco products to minors could be effective.
Opportunities
-
The findings suggest that smoking is considered a social behavior, particularly in work settings, during social drinking, or when gathering with friends. Smoking habits are closely intertwined with daily social activities, and these social activities and smoking habits serve as significant barriers to smoking cessation. People around them may either facilitate smoking by offering cigarettes, persuading others to smoke, or promoting the behavior. Conversely, material opportunities to quit smoking can be enhanced through partnerships, monitoring, guidance, understanding, and support[30].
Family influence plays a significant role in both smoking behavior and smoking cessation. Some participants mentioned that the expectations and encouragement from their family members were important motivators for quitting smoking. On the other hand, some participants also expressed that the smoking behavior of their family members posed a certain barrier to their smoking cessation efforts. This study emphasizes the importance of considering the family environment and the role of family members when designing smoking cessation interventions. Another qualitative study by Nagawa et al.[38] also confirmed this finding.
Motivations
-
We applied the BCW theory to explore both intrinsic and extrinsic motivation of smoking behavior and cessation. The internal motivation for smoking is curiosity about tobacco, the need to relieve stress, or simply to pass the time. For external motivation, many participants were influenced by people around them to start smoking and form a habit. Consequently, proper awareness of tobacco and smoke-free environments may be effective in stopping smoking.
Most of the participants mentioned that the extrinsic motivation for smoking cessation derives from public constraints or concerns about social image. Nevertheless, they believe the intrinsic motivation of quitting may be the key to successful smoking cessation, such as concerns for personal health and enhancing family relationships. Research has shown that pregnancy can act as a facilitator for smoking cessation among male partners[39]. In our study, we found that pre-pregnancy or childbearing-age women affected both men and women. There will be a powerful incentive to quit or reduce smoking during pregnancy or when trying to conceive.
Behavior
-
In this study, smoking and smoking cessation behaviors are the most crucial and notable factors influencing the success of quitting smoking. The behavior of smoking or smoking cessation is influenced by capability, opportunity, and motivation, and it also leads to the feedback effects. Research has revealed that smoking can become psychologically addictive[40]. Participants reported feeling anxious, restless, or irritable when they didn't have a cigarette, and they used smoking to relieve stress or create a sense of relaxation[41]. Emotions play an important role in smoking cessation. That is why Bupropion, a commonly known antidepressant, may aid smoking cessation[42]. When discussing quitting smoking, participants highlighted the importance of maintaining a positive mindset and having support from family and friends. This suggests that positive emotions, social support, and a sense of motivation play crucial roles in the quitting process.
Strengths and implications
-
This study employed a semi-structured qualitative interview approach to explore the barriers and facilitators to smoking cessation in Chinese people with a history of smoking. The research explored various aspects such as the reasons for starting to smoke, attitudes towards and awareness of smoking cessation, perceptions of the harmfulness of tobacco, knowledge of smoking cessation methods, and key factors influencing successful quitting. This comprehensive approach allows for a deeper understanding of the experiences of smokers and quitters across different age groups, shedding light on the barriers and facilitators encountered during smoking and quitting journeys.
In terms of the analysis theoretical framework, the BCW theory was applied to identify the determinants of implementation by detecting the barriers and facilitators to smoking cessation. As we coded and analyzed the data, we found that the barriers and facilitators for smoking cessation are in a complex interrelationship. Many of the factors were bi-directional for continuing or stopping smoking.
Firstly, participants were more likely to continue smoking when nicotine dependence was not considered a disease. Social situations can either promote or discourage smoking behaviour. People around can also increase the material opportunities for smoking by passing cigarettes, persuading, and promoting smoking. Material opportunities to stop smoking can also be increased through partnership, monitoring, leading, understanding, and support. These bidirectional socio-environmental factors provide more implications to help healthy people quit smoking.
Secondly, as an essential factor, personal emotion may promote smoking or prevent participants from stopping smoking. So for future clinical studies on smoking cessation interventions, we suggested that smoking cessation interventions should be combined with some psychological assistance. Additionally, traditional Chinese medicine may help relieve emotional stress[43,44].
Thirdly, the COVID-19 pandemic had an impact on both smoking and smoking cessation behavior. We identified several facilitators related to the COVID-19 pandemic: (1) the outbreak of COVID-19 has led to global health consciousness, which may prompt some smokers to recognize the importance of quitting smoking to improve their overall health and reduce their vulnerability to respiratory diseases; (2) the changes in social norms, such as the requirement of wearing masks in public places, has acted as a barrier to smoking; (3) the shift to remote work or staying at home limited the social opportunities for smoking. However, our research has also found that the stress, anxiety, and social isolation associated with the COVID-19 pandemic may further promote smoking behavior. A cross-sectional study conducted among adults in the United States indicated a decline in smokers' motivation to quit smoking during the pandemic[45].
Comparisons with previous studies
-
Previous qualitative studies in other countries have also examined the barriers and facilitators to smoking cessation. Consistent with our findings, these studies have identified factors such as shame, regulations, social aspect of tobacco use, nicotine addition, stress, limited understanding of the harms of smoking, and knowledge of cessation methods[46−52]. These findings resonate with our research, which also identified social and environmental influences as important determinants of smoking habits.
However, it is important to note some differences between our study and previous research. Some studies have focused on specific populations or health conditions or settings, such as pregnant women or smokers with Chronic Obstructive Pulmonary Disease (COPD), or primary care[48,53,54]. In this study, our research population consists of smokers without apparent pathological conditions, a group that is often genuinely capable of quitting smoking. Therefore, through interviews with the participants, we gain valuable insights into the cognitive processes and subjective perspectives of both smokers and quitters. This will enable us to provide universally applicable recommendations for smoking cessation.
Limitations
-
There are also some limitations to consider. Firstly, the sample size was relatively small, and there was a significantly smaller proportion of female participants compared to male participants. However, the gender proportion was roughly the same as in the 2018 Chinese Adult Tobacco Survey (male 50.5%, female 2.1%)[31]. Although the snowball sampling methods allowed us to access a diverse range of individuals, we acknowledge that it may have resulted in a non-representative sample and introduced selection bias.
Secondly, due to the impact of the COVID-19 pandemic, most interviews had to rely on online methods, which introduced certain limitations. The absence of face-to-face interviews may lead to some information bias or misinterpretation of the participants' responses. In addition, we could not separate the potential influence of the pandemic on smoking and smoking cessation behavior.
Thirdly, there were no restrictions in participating regarding age, sex, occupation, or geographical location. Though findings may have been limited for certain groups. Further research should prioritize large-scale cross-sectional studies to determine and validate the extent to which these barriers and facilitators influence smoking cessation.
-
Our findings revealed a strong association between smoking cessation and the social environment, as well as individual's knowledge, beliefs regarding health, motivations, and tobacco control policies. Given this study was conducted during the COVID 19 pandemic, additional research is needed to corroborate and generalize these findings for the development of effective smoking cessation interventions.
Much appreciation goes to all interviewees who shared their experiences and thoughts on smoking. This work was supported by the National Key Research and Development Project: adding Chinese herbal medicine to antibiotic treatment for acute exacerbation of chronic obstructive pulmonary disease (Grant No. 2018YFE0102300). JPL, CLL, and XHL were supported by Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (No: ZYYCXTD-C-202006). CLL was supported by Guangzhou Municipal Science and Technology Bureau (2024A04J4734). JPL was supported by High-level traditional Chinese medicine key subjects construction project of National Administration of Traditional Chinese Medicine—Evidence-based Traditional Chinese Medicine (zyyzdxk-2023249). NR is the guest professor of Beijing University of Chinese Medicine (Certification No. 20210017).
-
This study was approved by the medical ethics committee of the Beijing University of Chinese Medicine, Beijing, China (2021BZYLL03010). All participants in this study provided written consent to participate. Before their involvement, they received an overview of this study and were reassured about the strict confidentiality and anonymous nature of their participation.
-
The authors confirm contribution to the paper as follows: idea and conceptualization, methodology guidance: Lu CL, Liu JP; interview outline design and improment: Lu CL, Liu XH, Qiao SY; did the interviews: Qiao SY; data transcribed, coded the records and data analyzed: Lu CJ, Qiao SY, Zheng RX, Wang QY, Chen XY, Wei XH; writing - drafted manuscript preparation: Lu CL, Zheng RX, Wang QY, Pan XR; visualized the coding: Zheng RX, Lu CL; writing - manuscript revision: Liu JP, Robinson N, Liang LR, Xue X. All authors reviewed the results and approved the final version of the manuscript.
-
Single transcription cannot be shared considering the participants privacy, but the coding can be accessed in the supplementary files.
-
The authors declare that they have no conflict of interest.
- Supplementary Table S1 Basic demographic information of 30 interviewees.
- Supplementary Table S2 Codes and examples of the transcribed text from 30 interviewees.
- Copyright: © 2025 by the author(s). Published by Maximum Academic Press, Fayetteville, GA. This article is an open access article distributed under Creative Commons Attribution License (CC BY 4.0), visit https://creativecommons.org/licenses/by/4.0/.
-
About this article
Cite this article
Lu CL, Wang QY, Zheng RX, Pan XR, Chen XY, et al. 2025. Barriers and facilitators to smoking cessation in smokers: a semi-structured and qualitative interview. Journal of Smoking Cessation 20: e005 doi: 10.48130/jsc-0025-0005
Barriers and facilitators to smoking cessation in smokers: a semi-structured and qualitative interview
- Received: 04 December 2024
- Revised: 22 March 2025
- Accepted: 22 May 2025
- Published online: 30 May 2025
Abstract: Smoking remains a significant public health concern in China, with a high prevalence of tobacco use. This qualitative study aimed to explore the facilitators and barriers to smoking cessation among Chinese people with a history of smoking. A total of 30 Chinese individuals with diverse ages and professions, who self-reported a smoking history, participated in both one-on-one online video interviews, and face-to-face offline semi-structured interviews. The transcripts of all interview sessions were imported into Nvivo to facilitate thematic coding and subsequent theme analysis. The collected data was analyzed using the framework-theme analysis approach based on the Behavior Change Wheel (BCW) theory, resulting in categorization of codes and basic themes into four sub-themes: capability, opportunity, motivation, and behavior (COM-B). The age range of the participants was 13 to 63 years, with a distribution of 25 males and five females. On average, they had been smoking for 18.15 years. The findings indicate that the social environment plays a significant role in smoking cessation, as participants acknowledged the influence of family support, supervision, and companionship. Negative emotions such as anxiety and depression were identified as barriers to quitting smoking. Additionally, individual motivations related to personal health concerns and family responsibilities emerged as key drivers for tobacco cessation. Participants also recognized the impact of government legislation and school regulations in preventing teenagers from initiating smoking habits. However, there was a notable lack of awareness regarding the availability and benefits of smoking cessation clinics. The present study underscores the intricate factors influencing Chinese individuals' desire to quit smoking. To develop effective strategies for disseminating information about smoking cessation clinics, implementation research should prioritize addressing social environmental factors, which serve as pivotal determinants.