-
Indonesia has one of the highest tuberculosis (TB) burdens in the world, with 312 cases per 100,000 population in 2019 and a mortality rate of 34 per 100,000 population among those not infected with HIV. In addition, Indonesia contributes to the global increase in newly diagnosed TB cases, with a 69% increase from 2015 to 2019[1]. Globally, TB remains the leading cause of death from infectious diseases, with an estimated 1.7 billion people, or nearly a quarter of the world's population, infected with Mycobacterium tuberculosis in its latent form[2].
TB weakens the immune system, increasing susceptibility to opportunistic infections such as pulmonary aspergillosis. Prolonged treatment with antibiotics or immunosuppressive agents, as well as prolonged tuberculosis (TB) treatment, makes TB patients highly vulnerable to fungal infections, particularly those caused by Aspergillus fumigatus[3]. This condition can progress to chronic pulmonary aspergillosis (CPA), commonly occurring in post-TB patients as the fungus exploits lung damage and immune dysfunction[4]. In Indonesia, it is estimated that there are approximately 83,000 cases of CPA, with 17,561 new post-TB CPA cases annually[1]. CPA worsens TB treatment outcomes, causes progressive pulmonary fibrosis, and increases mortality if not promptly diagnosed[5,6].
Standard diagnostic methods, such as chest X-rays and sputum cultures, have limitations in detecting pulmonary aspergillosis promptly. Therefore, alternative strategies, such as serum Aspergillus IgG detection using Lateral Flow Assay (LFA) technology, such as LDBio Aspergillus, can potentially improve CPA diagnosis with rapid and accurate results. This LFA has shown better results in patients with a history of tuberculosis, making it suitable for use in TB-endemic countries like Indonesia for point-of-care diagnosis[7].
-
This study uses an observational analytic design with a cross-sectional approach. Data were obtained from both primary and secondary sources from post-tuberculosis (TB) patients receiving treatment at the pulmonary outpatient clinic of Dr. Saiful Anwar General Hospital, East Java, Indonesia. The study population included post-TB patients attending the outpatient clinic at Dr. Saiful Anwar General Hospital (Indonesia).
Inclusion criteria for the study were male or female patients over 18 years of age, post-tuberculosis patients confirmed by a negative rapid molecular sputum test (TCM) or negative acid-fast bacilli (AFB) smear on two occasions, and patients presenting with at least one of the following clinical symptoms: cough, hemoptysis, shortness of breath, fatigue, chest pain, or unexplained weight loss for more than 3 months, and patients with cavitary lesions (supported by radiological evidence). Patients willing to participate and sign the informed consent form were included.
Exclusion criteria included HIV-positive patients, pregnant patients, patients who had received systemic antifungal therapy in the last month, and severely immunocompromised patients (e.g., those with severe illness, cancer patients undergoing chemotherapy, patients with severe autoimmune diseases, or organ transplant recipients).
The study period was from May 2024 to February 2025. Sample collection and patient examination (anamnesis and physical examination) were conducted at the pulmonary outpatient clinic of Dr. Saiful Anwar General Hospital. The LD-Bio kit, specific Aspergillus IgG antibody levels, and sputum culture testing were performed at the Biomedical Laboratory, Faculty of Medicine, Brawijaya University, Malang (Indonesia).
The diagnosis of Chronic Pulmonary Aspergillosis (CPA) in this study refers to the official guidelines from the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), the European Respiratory Society (ERS), and the Infectious Diseases Society of America (IDSA).
The diagnostic criteria include: (1) chronic respiratory symptoms lasting ≥ 3 months, such as cough, hemoptysis, or dyspnea; (2) radiological findings consistent with CPA, such as cavitary lesions or nodules; (3) microbiological evidence such as positive sputum culture for Aspergillus spp. or reactive serology/galactomannan tests; and (4) histopathological confirmation through identification of Aspergillus hyphae in lower respiratory tract tissue.
Patients are categorized as probable CPA if they meet the first three criteria without histopathological confirmation, whereas proven CPA is established when all four criteria are fulfilled.
The clinical symptoms used in this study include chronic cough, dyspnea, hemoptysis, chest pain, and fatigue. Radiological findings consistent with CPA include pulmonary cavitation, aspergilloma, or persistent consolidation or nodules. The laboratory examinations used were sputum fungal culture and detection of Aspergillus antibodies using an enzyme-linked immunosorbent assay (ELISA) test. The LD Bio ICT result was not used in the diagnostic criteria, as it was the index test being evaluated in this study.
The LD Bio Aspergillus ICT is a rapid lateral flow immunochromatographic assay that detects antibodies (IgG and IgM) against Aspergillus spp. in serum. The test is performed by adding 20 µL of serum and four drops of buffer into the sample well. Results are read after 20–30 min. A visible band at the test line (T), along with a control line (C), indicates a positive result. The test is considered harmful if only the control line appears and invalid if the control line fails to appear.
The Aspergillus IgG ELISA was performed using a commercial kit (Bordier Affinity Products SA, Bâtiment Biokema, Chatanerie 2, 1023 Crissier, Switzerland; Lot No. 2417A-R). The assay is based on the enzyme-linked immunosorbent principle, where serum antibodies bind to Aspergillus antigens coated on microplate wells. After washing, enzyme-conjugated secondary antibodies are added, followed by the addition of substrate. The intensity of color change is measured at 450 nm using a microplate reader. Results are interpreted according to the manufacturer's cut-off values: < X units = negative, ≥ Y units = positive.
Sputum samples were cultured on Sabouraud dextrose agar and incubated at 25–30 °C for up to 7 d. Fungal growth was identified macroscopically by colony morphology and microscopically using lactophenol cotton blue staining. The culture was considered positive if Aspergillus spp. or other fungi grew and were morphologically identified. Species identification was performed when possible using visual and microscopic criteria.
Fungal identification at the species level was based on a combination of macroscopic colony morphology and microscopic characteristics. Colonies were evaluated for texture, pigmentation, and growth rate. Microscopic features such as hyphae, conidiophores, vesicle shape, and spore arrangement were examined. Identification was made through comparison with standard morphological keys and published atlases. No molecular methods were used in this study.
Data collected included sample characteristics such as age, gender, duration of TB treatment, comorbidities, and clinical symptoms. Diagnostic test results from LD-Bio ICT and Aspergillus IgG were analyzed using a 2 × 2 table, with sputum culture as the gold standard. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated.
Clinical symptom data for patients classified as probable CPA or non-CPA will be analysed using the Chi-Square test with a 95% confidence level and an alpha level of 0.05, where p < 0.05 is considered statistically significant.
-
This research was conducted at the outpatient clinic of Dr. Saiful Anwar General Hospital with 29 research subjects. The study's population comprises post-tuberculosis patients undergoing treatment at the clinic who meet the inclusion criteria. The demographic characteristics of the research sample are presented in Table 1.
Table 1. Research sample characteristics and bivariate analysis results based on CPA incidence.
Characteristics Probable CPA (n = 16) Non-CPA (n = 13) p-value N Percentage Mean ± SD N Percentage Mean ± SD Gender Men 10 34.5% 10 34.5% 0.404 Women 6 20.7% 3 10.3% Age (year) 51.88 ± 13.64 53.54 ± 14.86 0.756 TB treatment duration (month) 12.0 ± 8.41 10.23 ± 5.63 0.640 Comorbid Asthma 0 0 1 3.4% 0.259 COPD 2 6.9% 0 0 0.186 Diabetes mellitus 2 6.9% 1 3.4% 0.672 Lung cancer 1 3.4% 0 0 0.359 Malignancies other than lung 1 3.4% 0 0 0.359 Arthritis 1 3.4% 1 3.4% 0.879 Smoking history 5 17.2% 9 31.0% 0.042 Symptoms Cough with sputum 12 41.4% 10 34.5% 0.904 Hemoptysis 10 34.5% 8 27.6% 0.958 Chest pain 13 44.8% 8 27.6% 0.238 Shortness of breath 10 34.5% 11 37.9% 0.185 Unusual fatigue 15 51.7% 11 37.9% 0.422 Table 1 presents the characteristics of 29 study samples, comprising 20 males (69%) and nine females (31%). The average age of the samples is 52.62 years, with a weight of 51.12 kg, height of 160.21 cm, BMI of 19.83 kg/m2, and an average TB treatment duration of 11.21 months. Comorbidities identified include asthma (3.4%), chronic obstructive pulmonary disease (COPD, 6.9%), diabetes mellitus (10.3%), lung cancer (3.4%), non-lung malignancies (3.4%), arthritis (6.9%), and a history of smoking (48.3%). No samples had hypertension. 55.2% of post-tuberculosis patients were diagnosed with chronic pulmonary aspergillosis (CPA).
Table 1 shows no significant differences between the probable CPA and non-CPA groups in terms of gender, age, treatment duration for TB, and comorbidities (p-value > 0.05). The average age of patients with probable CPA was 51.88 years, while in the non-CPA group, it was 53.54 years. The proportion of male patients in both groups was the same (34.5%), but the proportion of females was higher in the CPA group (20.7%) compared to the non-CPA group (10.3%). The average treatment duration for TB was 12 months for the CPA group and 10.23 months for the non-CPA group. The prevalence of comorbidities such as COPD, diabetes mellitus, lung cancer, arthritis, and smoking history was higher in the non-CPA group (31.0%) compared to the CPA group (17.2%). The smoking history was significantly lower in the non-CPA group (p = 0.042). Common symptoms in CPA patients included cough (41.4%), productive cough (34.5%), hemoptysis (34.5%), chest pain (44.8%), shortness of breath (34.5%), and fatigue (51.7%). In the non-CPA group, similar symptoms occurred at slightly lower frequencies: cough (34.5%), productive cough (27.6%), hemoptysis (27.6%), chest pain (27.6%), shortness of breath (37.9%), and fatigue (37.9%). No significant differences were found between the two groups (p-value > 0.05).
-
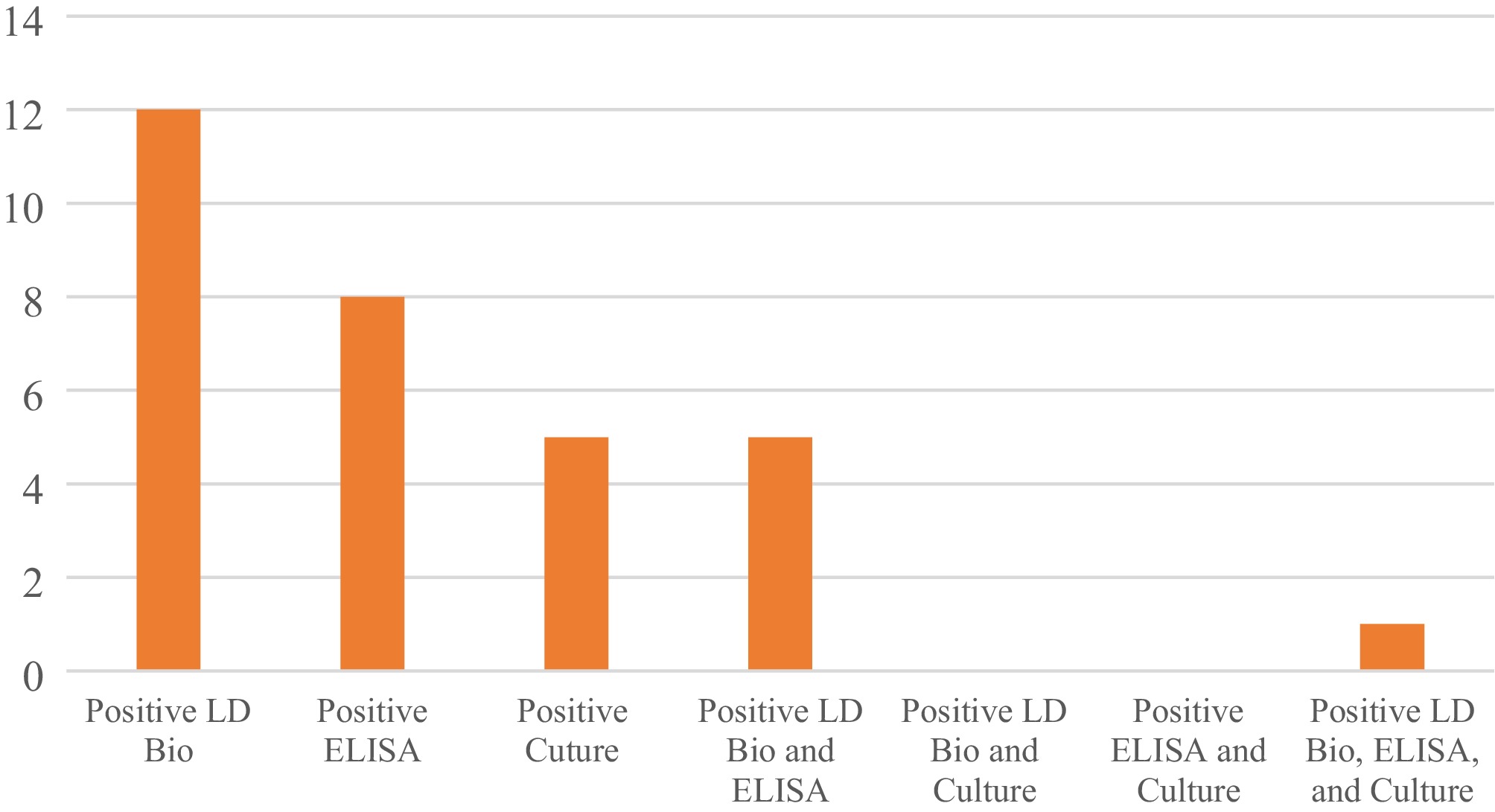
This study conducted a diagnostic test by examining samples using fungal sputum culture, serological testing with Aspergillus-specific IgG (ELISA), and an LD-Bio ICT check.
Figure 1 shows a positive LD-Bio ICT value in 12 patients (41.4%). The positive IgG Aspergillus (ELISA) value and positive fungal sputum culture were 17.2% and 27.6%, respectively. The incidence of positive CPA based on the three tests was found in only one patient or approximately 3.4%.
Among the positive fungal cultures, the identified species included Aspergillus niger, Aspergillus fumigatus, Aspergillus flavus, Candida sp., and Penicillium sp. Aspergillus fumigatus was the most frequently isolated species among patients with probable chronic pulmonary aspergillosis (CPA). These results highlight the predominance of fungal species commonly implicated in CPA among post-TB individuals. Figure 2 illustrates the typical colony morphology of Aspergillus fumagatus isolated from one of the patient specimens in this study.
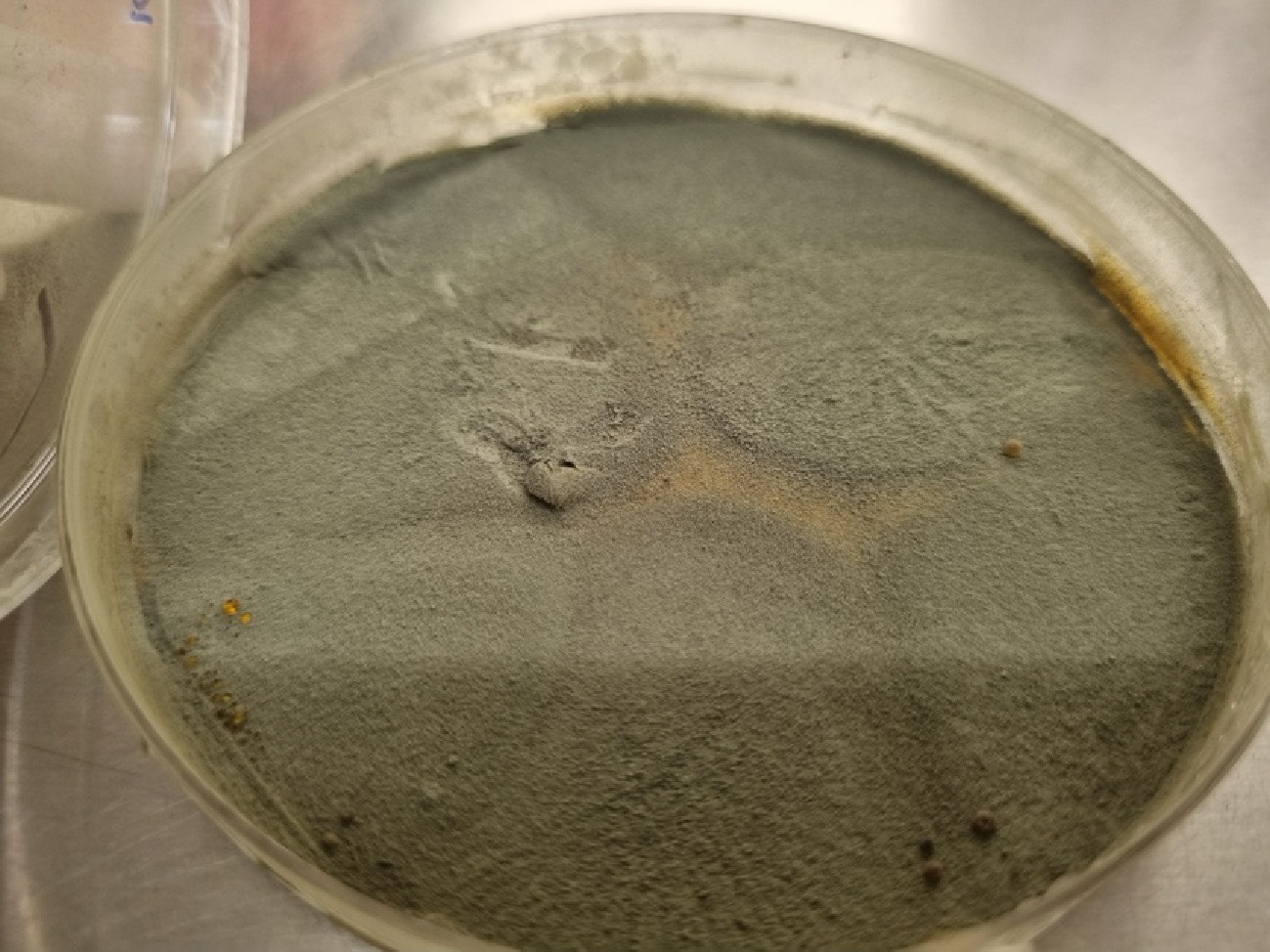
Figure 2.
Morphology of Aspergillus fumigatus colony grown on Sabouraud dextrose agar, showing bluish-green surface and velvety texture, consistent with the typical features of this species.
In this study, diagnostic tests for Chronic Pulmonary Aspergillosis (CPA) were performed using sputum culture as the gold standard. The diagnostic test results, obtained using the immunochromatographic test (ICT), are presented in Table 2. The enzyme-linked immunosorbent assay (ELISA) results are shown in Table 3.
Table 2 shows the diagnostic test results using ICT to detect probable CPA. The table includes data on the number of patients detected as positive and negative for probable CPA using ICT, as well as calculations of sensitivity, specificity, positive predictive value, negative predictive value, and test accuracy. Among the 29 patients tested, 12 patients diagnosed with CPA (41.4%) were detected as positive by ICT, while ICT did not detect four patients with probable CPA (13.8%). Conversely, among the 13 patients without CPA, one patient (7.7%) was detected as positive by ICT, and 12 patients (92.3%) were detected as unfavorable by ICT. The sensitivity of the ICT is 75.0%, indicating the test's ability to correctly identify patients with probable chronic pain syndrome (CPA) with a high degree of accuracy. The test's specificity is 92.31%, reflecting the test's ability to identify patients who do not have CPA.
Table 2. Diagnostic test of an immunochromatographic test for chronic pulmonary aspergillosis.
Diagnostic Probable CPA Sensitivity Specificity Positive predictive value Negative predictive value Accuracy Yes No ICT Positive 12 (41.4%) 1 (3.4%) 75.0% 92.31% 92.31% 75.0% 82.76% Negative 4 (13.8%) 12 (41.4%) Bold values indicate positive predictive value and accuracy as key diagnostic parameters. Table 3 shows the diagnostic test results using ELISA to detect CPA. This table presents data on the number of patients detected as positive and negative for CPA using ELISA, along with calculations of the test's sensitivity, specificity, positive predictive value, and negative predictive value. Among the 29 patients tested, eight patients diagnosed with CPA (27.6%) were detected as positive by ELISA, while ELISA did not detect eight patients with probable CPA (27.6%). Conversely, among the 13 patients without CPA, three patients (23.1%) were detected as positive by ELISA, and 10 patients (76.9%) were detected as unfavourable by ELISA. The sensitivity of ELISA is 50.0%, indicating the test's ability to detect patients with probable CPA. The test's specificity is 76.92%, reflecting the test's ability to identify patients without CPA. The positive and negative predictive values are 72.73% and 55.56%, respectively, showing the test's accuracy in correctly identifying patients who are positive and negative for CPA. These results indicate that ELISA has lower specificity and sensitivity than ICT, suggesting that ELISA may be less reliable than ICT in detecting CPA. The accuracy of ICT at 82.76% shows that the ICT method correctly identified cases in 82.76% of all trials conducted. In comparison, the accuracy of ELISA at 62.07% indicates that the ELISA method has a lower success rate, correctly identifying only 62.07% of cases. This suggests that ICT performs better than ELISA in the context of the tests conducted.
Table 3. Diagnostic test of enzyme-linked immunosorbent assay for chronic pulmonary aspergillosis.
Diagnostic Probable CPA Sensitivity Specificity Positive predictive value Negative predictive value Accuracy Yes No ELISA Positive 8 (27.6%) 3 (10.3%) 50.00% 76.92% 72.73% 55.56% 62.07% Negative 8 (27.6%) 10 (34.5%) Bold values indicate positive predictive value and accuracy as key diagnostic parameters. Table 4 presents the diagnostic test results using the immunochromatographic test (ICT) in comparison to sputum culture for the diagnosis of chronic pulmonary aspergillosis (CPA). ICT shows a sensitivity of 40%, a specificity of 54%, a positive predictive value of 15%, and a negative predictive value of 81%. Among all tests conducted, the accuracy of ICT in detecting CPA is approximately 52%.
Table 4. Diagnostic test of an immunochromatographic test against sputum culture results for chronic pulmonary aspergillosis.
Diagnostic Culture Sensitivity Specificity Positive predictive value Negative predictive value Accuracy Yes No ICT Positive 2 (6.9%) 11 (37.9%) 40.00% 54.17% 15.38% 81.25% 51.72% Negative 3 (10.3%) 13 (44.8%) Bold values indicate positive predictive value and accuracy as key diagnostic parameters. Table 5 presents the diagnostic test results using ELISA in comparison to sputum culture for the diagnosis of CPA. ELISA shows a sensitivity of 40%, a specificity of 63%, a positive predictive value of 18%, and a negative predictive value of 83%. The overall accuracy of ELISA in detecting CPA is approximately 59%. These results indicate that ELISA has higher specificity compared to ICT.
Table 5. Diagnostic test of enzyme-linked immunosorbent assay against sputum culture results for chronic pulmonary aspergillosis.
Diagnostic Culture Sensitivity Specificity Positive predictive value Negative predictive value Accuracy Yes No ELISA Positive 2 (6.9%) 9 (31.0%) 40.00% 62.50% 18.18% 83.33% 58.62% Negative 3 (10.3%) 15 (51.7%) Bold values indicate positive predictive value and accuracy as key diagnostic parameters. -
This study shows that most post-tuberculosis patients are male, and 55.1% suffer from probable CPA. CPA occurs due to an Aspergillus infection that takes advantage of lung damage caused by tuberculosis, leading to cavities, fibrosis, and aspergillomas, which exacerbate the already compromised lung condition[5]. These findings are higher than those reported in the study by Rozaliyani et al.[1], which showed that 20 out of 90 post-tuberculosis patients suffered from CPA. However, Neuböck et al.[8] indicated that around 50% of post-tuberculosis patients develop CPA after completing tuberculosis treatment.
The average age of patients in this study was 52.62 years, consistent with previous studies that have shown a higher prevalence of CPA in older patients. In Vietnam, the average age of CPA patients is 59 years[5]; in Pakistan, it is 45.75 years[9]; and in France, it is 65 years[10]. This suggests that CPA is more frequently found in older patients, especially those with a history of lung diseases such as tuberculosis.
The duration of TB treatment did not show a significant difference between probable CPA and non-CPA patients. Previous research by Ocansey et al.[11] showed that a longer duration of TB treatment is associated with more severe lung damage and cavity formation, which provides an ideal environment for Aspergillus growth. In Ghana, the incidence of CPA in TB patients was recorded at 3.3% at the end of treatment and increased to 7.4% six months after treatment completion. In Indonesia, the prevalence of CPA has risen from 6% at the beginning of TB treatment to 8% at the end of therapy[12].
The comorbidity of diabetes mellitus (DM) was found in 10% of patients in this study, although no significant difference was observed between the groups. Previous research indicates that patients with DM have a higher risk of developing CPA. Diabetes mellitus can cause immune system dysfunction, making patients more susceptible to fungal infections, such as those caused by Aspergillus. A study in Indonesia found that around 28.4% of CPA patients also had diabetes[13]. Other research shows that diabetic patients with CPA often exhibit more severe symptoms and have a worse prognosis, including higher mortality rates and the need for intensive care[9]. No significant difference was found in clinical symptoms between post-tuberculosis patients with and without CPA. Previous studies have shown that clinical symptoms such as cough, productive cough, hemoptysis, chest pain, shortness of breath, and fatigue were nearly equal in patients with and without CPA[8,14].
In this study, the classification of probable CPA was based on a combination of clinical symptoms, radiological findings, and positive results from LD Bio ICT, Aspergillus IgG ELISA, or sputum fungal culture. Therefore, the evaluation of LD Bio ICT performance against this classification may reflect its role in the diagnostic process. To complement this, we also conducted an independent analysis comparing LD Bio ICT and ELISA results directly to sputum culture as the reference standard.
The formation of cavities in tuberculosis involves the interaction between Mycobacterium tuberculosis and the body's immune response, leading to cavities that serve as bacterial reservoirs[14]. Cavities in aspergillosis, particularly chronic pulmonary aspergillosis (CPA), form due to the interaction of Aspergillus with the immune system, especially in individuals with a history of lung diseases, such as tuberculosis. Aspergillus colonises damaged lung tissue, utilising the necrotic environment for its growth and spread[14].
Inflammation in aspergillosis involves the activation of macrophages and neutrophils, which release pro-inflammatory cytokines, including tumour necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1β (IL-1β). These cytokines play a role in recruiting immune cells to the site of infection but are often insufficient to eliminate the fungus. Additionally, matrix metalloproteinases (MMPs), particularly MMP-9 and MMP-12, play a role in the degradation of the extracellular matrix in the lungs, accelerating tissue destruction and enlarging cavities[15]. Cavities in aspergillosis have thick walls composed of fibrin and necrotic tissue, which become sites for the formation of aspergillomas. These cavities often become a source of chronic infection that is difficult to treat, worsening inflammation and stimulating further growth of Aspergillus.
The use of ICT and ELISA in the diagnosis of CPA
-
This study reveals that LD Bio has the highest positive value at 41.4% and has the potential to serve as a screening tool for CPA. A positive incidence of CPA was found in only one patient, approximately 3.4%[16]. Immunochromatography works faster than culture, providing results in minutes, whereas culture requires incubation times of 24 to 72 h. Therefore, culture is not suitable for CPA screening.
LD Bio-ICT has a sensitivity of 75.0% and a specificity of 92.31%, indicating its effectiveness in detecting CPA with relatively low error rates. This suggests that ICT LD-Bio is effective in identifying patients without CPA and detecting most infected patients. In contrast, ELISA IgG Aspergillus shows a sensitivity of 50.0% and a specificity of 76.92%, which is lower than that of ICT. The lower sensitivity means some CPA cases may go undetected, potentially delaying diagnosis and proper treatment. However, ELISA remains a valid tool, particularly when used in conjunction with other diagnostic tests to enhance accuracy and specificity.
Previous studies have also evaluated various diagnostic tests for CPA, as seen in the study by Page et al.[17], who found that ImmunoCAP and Immulite had the highest sensitivity and specificity at 96% and 98%, respectively. Takazo & Izumikawa[18] found a sensitivity of 62% and specificity of 67.7% in the AspLFD test, while Li et al.[19] reported a sensitivity of 84.1% and specificity of 89.6% in the Aspergillus-specific IgG test[18,19]. Sehgal et al.[20] found a sensitivity of 95.6% and specificity of 100% in the Aspergillus fumigatus-specific IgG test, while Shin et al.[21] found a sensitivity of 23% and specificity of 85% in the serum galactomannan antigen test[20].
This study has several limitations. First, it was conducted at only RSSA, resulting in a small sample size. With such a limited sample, it is challenging to generalize the findings to a broader population. Second, this study did not utilise histopathology and bronchoalveolar lavage which are considered as the gold standards for diagnosis.
Implications for screening strategy in TB-endemic settings
-
This study is not the first in Indonesia to evaluate the use of immunochromatographic testing (ICT) for the diagnosis of chronic pulmonary aspergillosis (CPA). Previously, Rozaliyani et al.[1] conducted a study using a combination of Western Blot (WB) and ICT, which demonstrated that ICT is effective as a screening tool. At the same time, WB serves as a confirmatory test and may also provide insight into disease severity.
In contrast to that study, our research directly compares three diagnostic methods: LD Bio ICT, Aspergillus IgG ELISA, and sputum fungal culture. Although ICT has been widely used in other countries, its application in Indonesia remains limited. Therefore, this study is expected to make a significant contribution to the adoption of ICT as a rapid, practical, and effective diagnostic tool for use in tuberculosis-endemic settings, such as Indonesia.
Moreover, this study demonstrates the implementation of LD Bio ICT in a real-world outpatient setting in a high tuberculosis (TB)- burden country, particularly Indonesia. While LD Bio ICT is already well-established internationally as a simple and rapid screening tool for CPA, evidence of its use in daily clinical practice in Indonesia remains scarce. Our findings provide preliminary data supporting the effective use of LD Bio ICT in referral healthcare facilities located in TB-endemic areas, with substantial potential to support national CPA screening programs.
Our results showed that LD Bio ICT achieved a sensitivity of 75% and a specificity of 92.31%, outperforming the Aspergillus IgG ELISA, which had a sensitivity of 50% and a specificity of 76.92%. Although sputum culture had very high specificity (100%), its sensitivity was low (31.25%), making it less suitable as a screening tool. Therefore, LD Bio ICT could serve as a more practical and efficient alternative for early CPA detection, especially in primary healthcare settings that require accessible, rapid, and simple diagnostic methods in high TB-burden regions, such as Indonesia.
This study has some limitations that should be acknowledged. First, the diagnostic reference standard did not include histopathological examination of lung tissue or fungal culture from bronchoalveolar lavage fluid, which are considered gold standards for confirming CPA, typically requiring histopathological demonstration of Aspergillus hyphae or a positive culture from a sterile site, such as lung tissue or bronchoalveolar lavage fluid (BALF)[22]. Although the findings provide valuable insights, further studies are needed to validate the results in broader and more diverse populations, thereby improving generalizability. The study involved collaboration with an external centre (Parasitology Laboratory, Faculty of Medicine, Universitas Indonesia), necessitating specimen transport across locations, which could impact the timeliness and stability of sample handling.
-
Based on the comparison between LD Bio-ICT, IgG aspergillosis, and fungal culture in confirming probable CPA, it can be concluded that LD Bio-ICT has higher sensitivity in post-tuberculosis patients with probable CPA, with the highest positive value of 41.4%. There were no differences in chronic symptoms, such as cough, coughing up blood, shortness of breath, and fatigue, among these patients. LD Bio-ICT demonstrated 82.76% accuracy, 75% sensitivity, and 92.31% specificity, whereas Aspergillus IgG ELISA achieved 62.7% accuracy, 50% sensitivity, and 76.92% specificity. To support these findings, further research is recommended, including the evaluation of diagnostic tests using histopathology and bronchoalveolar lavage as the gold standard for comparison. Furthermore, future studies should involve a larger sample size and include research centers from various regions to improve the generalizability of the results.
-
The authors confirm their contribution to the paper as follows: writing - original draft: Fahmi K; conceptualization: Fahmi K, Pratiwi SD; methodology: Fahmi K, Setijowati N; data collection: Sugiri YJR; analysis, interpretation of results: Sugiri YJR, Pratiwi SD; validations: Setijowati N; supervision and writing-review & editing: Rozaliyani A. All authors reviewed the results and approved the final version of the manuscript.
-
The data supporting the findings of this study are not publicly available due to patient privacy and institutional regulations but are available from the corresponding author upon reasonable request.
-
The authors thank Dr. Saiful Anwar General Hospital, East Java, Indonesia, for facilitating this research.
-
The authors declare that they have no conflict of interest.
- Copyright: © 2025 by the author(s). Published by Maximum Academic Press, Fayetteville, GA. This article is an open access article distributed under Creative Commons Attribution License (CC BY 4.0), visit https://creativecommons.org/licenses/by/4.0/.
-
About this article
Cite this article
Fahmi K, Sugiri YJR, Pratiwi SD, Setijowati N, Rozaliyani A. 2025. LD BIO-ICT system non-inferior to Aspergillus IgG and fungal culture in the diagnosis of probable chronic pulmonary aspergillosis (CPA). Studies in Fungi 10: e013 doi: 10.48130/sif-0025-0014
LD BIO-ICT system non-inferior to Aspergillus IgG and fungal culture in the diagnosis of probable chronic pulmonary aspergillosis (CPA)
- Received: 21 March 2025
- Revised: 21 June 2025
- Accepted: 23 June 2025
- Published online: 25 July 2025
Abstract: Chronic pulmonary aspergillosis (CPA) is a significant complication in post-tuberculosis (TB) patients, requiring accurate diagnosis for effective management. LD-Bio Immunochromatography (ICT) and Aspergillus IgG Enzyme-Linked Immunosorbent Assay (ELISA) are commonly used to detect Aspergillus infections. This observational analytic study, employing a cross-sectional design, was conducted among post-TB patients at Dr. Saiful Anwar General Hospital in East Java, Indonesia. Patients who met the criteria for probable CPA underwent sputum culture, Aspergillus IgG ELISA, and LD Bio ICT testing. The sensitivity and specificity of LD Bio ICT and Aspergillus IgG ELISA were evaluated using 2 × 2 tables in two separate analyses: one using probable CPA diagnosis as the reference, and another using sputum culture as an independent comparator. Twenty-nine patients were included, with 16 classified as probable CPA and 13 as non-probable CPA. LD-Bio ICT showed 75% sensitivity, 92.31% specificity, 92.31% positive predictive value, 75% negative predictive value, and 82.76% accuracy. In comparison, ELISA had a sensitivity of 50%, a specificity of 76.92%, a positive predictive value of 72.73%, a negative predictive value of 55.56%, and an accuracy of 62.07%. Sputum culture had 100% specificity and 31.25% sensitivity, with an overall accuracy of 62.07%. LD-Bio ICT outperforms the Aspergillus IgG ELISA in terms of sensitivity, specificity, and accuracy in diagnosing CPA in post-TB patients.
-
Key words:
- Antibody detection /
- Fungal infection /
- Immunochromatographic assay /
- Indonesia /
- Post-tuberculosis /
- Serological test