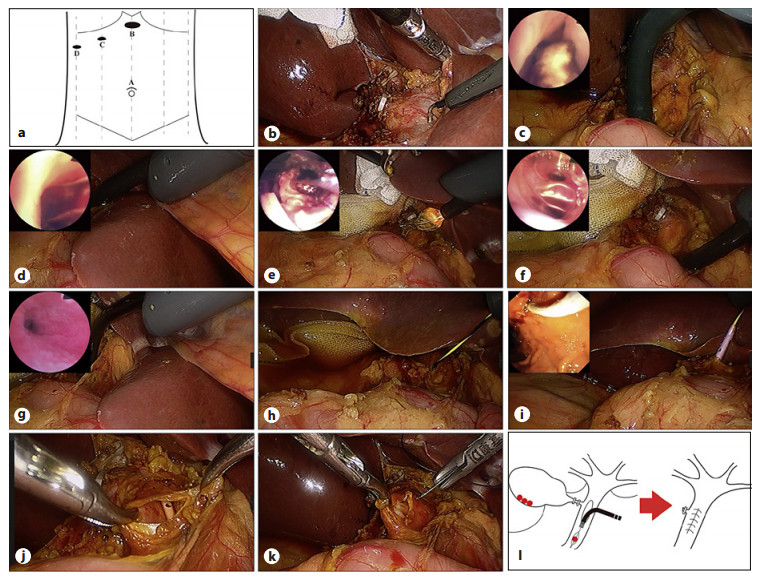
Background: Primary duct closure (PDC) after laparoscopic common bile duct exploration (LCBDE) has been widely applied for choledocholithiasis. However, there has been controversy over the placement of endoscopic nasobiliary drainage (ENBD) during operation. To date, few studies compare the clinical effect of PDC without and with ENBD. The aim of this study was to assess the safety and efficacy of PDC without ENBD for choledocholithiasis.
Methods: From January 2016 to December 2018, a total of 164 patients meeting the inclusion criteria were enrolled and divided into group A (undergone LCBDE + PDC without ENBD, 81 cases) and group B (undergone LCBDE + PDC with ENBD, 83 cases) in this study. The intraoperative conditions and postoperative complications were compared between the 2 groups.
Results: In group A, the time of operation, postoperative first flatus, extubation, antibiotics, and discharge were shorter than in group B (t = −17.775, p = 0.000; t = −7.649, p = 0.000; t = −5.807, p = 0.000; t = −9.247, p = 0.000; t = −9.322, p = 0.000, respectively). Furthermore, intraoperative blood loss was less (t = −2.199, p = 0.029) and hospital costs were lower (t = −6.685, p = 0.000). However, there was no significant difference in postoperative complications between the 2 groups (p > 0.05).
Conclusions: In patients who meet the screening criteria, PDC without ENBD after LCBDE is safe and effective and worthy of clinical application.